White coating on the tongue is usually perceived as a symptom of the disease. A person, as a rule, does not consider his language. In order for us to stand in front of the mirror, stick out our tongue and begin to look at it, there must be some reason that prompted us to do so - discomfort in the throat or oral cavity or some other dissatisfaction with our health. And then we discover a white coating on the tongue (or, as they sometimes say, that our tongue is coated ). However, don't be scared right away. Even a healthy person can have a white coating on the tongue. On the other hand, plaque on the tongue can indeed be a manifestation of the disease. Therefore, it is useful to know how pathological plaque on the tongue differs from plaque, which is considered a variant of the physiological norm.
Physiological white coating on the tongue
White coating on the tongue is most often found in the morning. At night, less saliva is produced, which contributes to the activation of bacterial activity. As a result, by morning, almost all people develop a white coating on their tongue. Sometimes it is accompanied by bad breath.
As a rule, such plaque is easily removed during morning oral hygiene. When we brush our teeth, it is advisable to also brush our tongue, especially its root. Modern toothbrushes have a surface specially modified for this purpose (the other side in relation to the bristles).
However, the white coating disappears on its own as the day begins. It is erased when eating, and the greater amount of saliva released prevents it from forming again.
How to clean your tongue
If you don't have any health problems that affect the plaque, just follow these guidelines and remember to brush until all the plaque is removed and your tongue is pink again. Typically, tongue hygiene takes only 20–30 seconds.
Recommendations for adults
- Proceed with the procedure only after brushing your teeth
and rinsing your mouth. - Use special tools
: scrapers, nozzles and others. - Clean your tongue using sweeping movements
and light pressure. - Start from the root of the tongue
and end with the tip. - Do not brush your tongue with cross movements and do not press
too hard - this can damage it. - Don't forget to clean the instrument
after the procedure. - Be sure to rinse your mouth
with water.
Should children have their tongues cleaned?
Children also need tongue care, but not earlier than 3–4 years.
For younger children, tongue cleaning is pointless. They don’t eat junk food, especially not in the same quantities as adults, and they don’t drink tea and coffee. Until 3–4 years of age, normal oral care is sufficient. From 3–4 to 8 years
This is how you should clean your tongue.
- Move from the root of the tongue to the tip
with smooth sweeping movements, with even weaker pressure than with adults. - Similarly, clean the sides
of the tongue and the inside of the cheeks. - Be sure to rinse your mouth
.
From the age of 8
you can already use scrapers.
Pathological plaque on the tongue
If the white coating on the tongue is caused by an illness, it persists throughout the day. A thin white coating occurs with any ARVI. It disappears as soon as the patient recovers.
Particular attention should be paid to the compaction of plaque. The body of the tongue is not visible through the thick coating. Such plaque is difficult to remove. Thick plaque is considered a sign indicating the severity of the disease.
The color of the coating on the tongue is also important. The more intense the color, the more serious the pathology that caused the plaque. The color of plaque is not only white. A yellowish tint to the plaque may be associated with a malfunction of the gallbladder or pancreas. Gray plaque is possible in case of stomach disease - gastritis, peptic ulcer. In some severe infectious diseases, plaque may acquire a black, bluish or greenish tint.
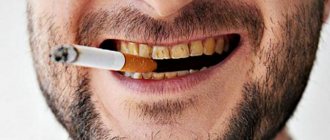
However, it should be taken into account that the color of plaque can be affected by smoking, drinking and eating.
What can cause pathological plaque?
The main reason is a malfunction of the internal organs. However, there are two other possibilities: smoking and improper oral hygiene. For active smokers, a yellowish coating is a constant companion, which may not indicate anything bad about health other than the presence of a bad habit. If you don't brush your mouth properly, your tongue will be completely ignored. It is wrong to brush your teeth alone. Bacteria accumulate on the surface of the tongue; they also need to be removed. To clean the tongue, many toothbrush manufacturers make a special brush on the other side. There are also scrapers for the surface of the tongue.
If a person does not smoke and maintains proper hygiene, but there is still plaque, then this may be an indicator of the following diseases:
- Diseases of the digestive system (the most common cause) are ulcers, gastritis, diseases of the gallbladder, pancreas, and liver. Usually in such cases the plaque is accompanied by a persistent unpleasant odor that does not go away even after cleaning.
- Diseases of the respiratory system - tuberculosis, bronchitis, asthma.
- Infectious diseases - influenza, sore throat, ARVI, acute respiratory infections.
- Reduced immunity.
- Diseases of teeth and gums.
- Changes in acid-base balance due to medications.
Diseases that cause plaque on the tongue:
- stomatitis;
- thrush (candidiasis). Caused by fungi of the genus Candida. The disease can be caused by long-term use of antibiotics or decreased immunity. With oral candidiasis, a typical manifestation is a dense milky-white coating that covers the tongue in spots. Similar spots may also appear on the roof of the mouth or gums. In severe cases, plaque covers the entire tongue as well as the walls of the throat, making swallowing and breathing difficult.
- scarlet fever. In the first days of the disease, the tongue is covered with a white-gray coating. Then the coating disappears, and the tongue acquires a crimson color;
- whooping cough. A pale yellowish coating on the tongue may be accompanied by bad breath;
- dysentery. A thick white coating is typical;
- cholera. Characterized by a dark coating (even black);
- diphtheria;
- gastritis;
- stomach ulcer;
- enterocolitis;
- pancreatitis;
- stomach cancer;
- kidney diseases;
- some other diseases.
What do different types of smell mean?
Unpleasant odors are caused by several types of volatile compounds produced by anaerobic bacteria. They use food debris on the tongue, between teeth and in carious cavities as a nutrient medium. Depending on the predominant compound, the character of the odor changes. Some of them suggest the pathology that caused halitosis:
- sour aroma – stomach diseases, gastritis or ulcers;
- feces, rotten cabbage - oral pathology, caries;
- smell of urine - kidney failure;
- the smell of ammonia or rotting apples – diabetes;
- rot, rotten meat - esophageal diverticulum.
You can find additional symptoms that will accurately indicate the cause of halitosis. If you have stomach pathology, you will experience pain between snacks. Diabetes mellitus is accompanied by excessive urination, dry mouth and thirst. Caries may not appear for a long time, but in advanced forms toothache appears.
Given the variety of causes, diagnosis, prevention and treatment of halitosis can be performed by doctors of different specialties. You need to see a dentist to get rid of dental diseases, but in other cases you will need to consult an endocrinologist, therapist or nephrologist.
When and which doctor to contact about a coating on the tongue
As a rule, tongue coating is not the main symptom.
And it is other symptoms that tell you which doctor you should see. If plaque on the tongue is accompanied by symptoms of ARVI, you should consult a physician. If you have symptoms of gastrointestinal diseases, contact a gastroenterologist. If there are no such symptoms, and the cause of your concern is plaque, in case of white plaque you can consult a dentist, in case of yellowish or gray plaque, you can consult a gastroenterologist. And in any case, you can consult a general practitioner - family doctor or therapist. A child with a persistent coating on the tongue should be shown to a pediatrician.
Professional cleaning of smoker's plaque
To remove smoker's plaque, the Air Flow method was used, in which a mixture of cleaning powder and water is applied to the teeth through a special nozzle under pressure. This cleaning method effectively removes plaque from all hard-to-reach places.
Hard plaque and tartar are removed using ultrasound. To restore the mineral composition of the enamel and increase its protective properties, apply Tuss Moose cream in a mouth guard to the teeth for 10 minutes.
Can a smoker get tongue cancer from smoking?
When smoking, the tongue is the first organ to take the hit of nicotine. With constant smoking, the organ receives microtraumas, which increase over time. Also, other formations that can develop into cancer may appear on the mucous membrane due to tobacco smoke.
IMPORTANT! Tongue cancer is dangerous because it can only be diagnosed in late stages, and it develops rapidly.
The first signs are the appearance of ulcers and seals. At the beginning of the disease, ulcers and seals have clear boundaries, but as it progresses, the boundaries are erased, and the edges rise upward and resemble rollers in appearance.
Over time, the smoker develops pain, swelling of the face, and difficulty opening the mouth and, accordingly, eating.
Uvula body cancer
The most common type of oncology. The malignant neoplasm affects the middle of the tongue, as well as its lateral parts.
Tongue root cancer
Root damage is characterized by severe pain when swallowing food. This type of oncology is less common compared to the previous one.
The disease also has a second name - oropharyngeal cancer. In this case, the tumor is located at the back of the mouth.
The pathological process is aggressive and treatment is extremely rare.
What dangers can plaque and untimely removal pose for a smoker?
We have already said that plaque is not only unsightly, but also dangerous. The formation of plaque indicates tissue destruction, and therefore a deterioration in the functionality of the organ. Its main function is taste sensitivity and transmission of further signals to the brain. If no signals were received, the body did not understand that the digestion process should begin. It is for this reason that digestive problems occur.
Also, plaque in a smoker is a sign of the presence of viruses and microbes that, with saliva, enter the internal organs through the mucous membrane. All harmful microorganisms continue to multiply in the body, disrupting the functioning of each organ separately.
Eliminating other causes of unpleasant odor
It is more difficult to get rid of bad breath that is not related to dentistry. If the cause is metabolic disorders, treatment may take a long time. With diabetes, it is important to achieve stable blood glucose levels. Then the ammonia aroma will not bother you. To do this, patients with type 1 disease carefully select the dosage of insulin, and for type 2 diabetes mellitus, they are prescribed a balanced diet and medications to lower blood glucose.
For those with severe kidney problems, the only way to eliminate the smell of urea is to undergo hemodialysis. This is a method of artificial purification of blood plasma, which helps get rid of metabolic products.
Treatment of tonsillitis and respiratory pathologies is carried out with antibiotics. But with the chronic course of the pathology, this is a long process.
The most common cause of bad breath is improper oral care. By visiting the dentist at least once a year and choosing the right brush, paste and floss, you can avoid the onset of halitosis or treat it at an early stage.
Features of a smoker's tongue
Smoking negatively affects the entire body of the smoker and those around him. However, the most noticeable sign of a smoker is often the tongue, which changes its appearance over the course of smoking. Even a novice doctor can easily distinguish between the mouth of a non-smoker and a smoker.
Nicotine affects the sensitivity of taste buds, causing food to taste worse. Taste buds are necessary for a person not only to sense a certain taste, but also to improve the process of salivation, digestion and the secretion of gastric juice. This means that smoking directly affects the condition of the tongue, and indirectly changes the digestion process, slowing it down.
A smoker’s plaque is not just an accumulation of microbes and harmful microorganisms, but a change in its entire structure.
Abstract | Cigarette smoking is inextricably linked with serious pathology of all systems of the human body, and the skin is no exception. The subject of this review is the harm that tobacco consumption causes to the skin. It is important to determine the difference between the effects of smoking and the effects of nicotine on the skin. All skin cells express several subtypes of nicotinic acetylcholine receptors (nAChRs), including the α7 receptor subtype. Smoking affects some chronic dermatoses negatively, while others have a positive effect. Having identified the negative impact of smoking on a certain disease, patients can be advised to quit it, and in the opposite cases, therapeutic agents based on nAChR agonists can be developed. Toxic components of tobacco products Cigarette smoking is inextricably linked with serious pathology of all systems of the human body, and the skin is no exception. Despite attempts to warn the population about the dangers of smoking, it remains a leading cause of preventable death. Tobacco smoking has been known in Europe since Christopher Columbus noticed the Arawak Indians smoking tobacco leaves in 1492. The tobacco plant was named Nicotiana tabacum in honor of the French ambassador to Portugal, who introduced France to this plant - Jean Nicot. Nicotine, the main alkaloid in tobacco, was isolated in 1828. Nicotine can enter the human body through smoke inhalation into the lungs or gastrointestinal tract, or through intranasal sprays, transdermal patches, topical creams, or enemas. Small amounts of nicotine are found in foods such as tomatoes, potatoes and eggplant. Nicotine can be absorbed into the bloodstream through the mouth, lungs, bladder, gastrointestinal tract, and skin. From 70 to 80% of nicotine absorbed in the gastrointestinal tract is converted into its most important metabolite, cotinine, during its first passage through the liver [1]. The rate of nicotine absorption through the skin and mucous membranes is directly dependent on its concentration. The half-life of nicotine is approximately two hours [2]. From a dermatological point of view, tobacco use carries many dangers to the skin, which can occur both through a direct effect on the epidermis and indirectly through the bloodstream. Tobacco smoke consists of a solid dispersed phase, which includes its main alkaloid - nicotine, as well as a volatile phase. It contains many mutagens and carcinogens, in particular polycyclic aromatic hydrocarbons (PAHs), nitrosamines and heterocyclic amines. The main toxic components of the solid phase include nicotine, phenol, catechol, quinoline, aniline, toluidine, nickel, N-nitrosodimethylamine, benzopyrene, benzanthracene and 2-naphthylamine. The main toxic components of the gas phase are carbon dioxide, carbon monoxide, hydrogen cyanide, nitric oxide, acetone, formaldehyde, acrolein, ammonium cations, pyridine, 3-vinylpyridine, N-nitrosodimethylamine and N-nitrosopyrrolidine. Gene expression studies in skin cells have shown that tobacco components activate the expression of 14 different genes involved in xenobiotic metabolism and response to oxidative or other stress [3]. The non-genomic effects of tobacco smoke are due to the formation of reactive oxygen species (ROS). Nicotine and its metabolites affect the skin through activation of nicotinic cholinergic receptors (nAChRs) expressed by epithelial cells [4]. Signs of smoking on mucous membranes and skin Heavy smokers, as a rule, can be identified by characteristic manifestations on the skin and mucous membranes. Yellow discoloration of light-colored mustaches and nails soaked in tobacco byproducts is often found. When smoking cessation occurs, a distinguishable boundary appears between the distal pigmented portion of the nail and the growing normal nail, a phenomenon known as the Harlequin nail or quitter nail (Figure 1). Based on the length of a normal nail that has grown, one can guess how long a person has not smoked. Chronic heat from a lit cigarette also stains the fingertips due to post-inflammatory hyperpigmentation. One third of smokers have noticeable perioral hyperpigmentation [5]. In children who passively inhale tobacco smoke [6], as well as consuming nicotine sublingually, gum pigmentation can be detected [7]. Pigmentation of the gums is caused by the formation of melanin granules synthesized in melanosomes. Nicotine, which can act as a precursor for melanin synthesis, can irreversibly bind to melanin and accumulate in melanin-containing tissues [8]. It is known that other components of tobacco, especially carcinogens such as N'-nitrosonornicotine (NNN), 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) and benzopyrene, accumulate in tissues containing melanin [9].
Figure 1 | Harlequin's nail or "one who is trying to get off"
(a) Nicotine staining and line of demarcation on several fingers. (b) A line of demarcation between the distal pigmented part of the nail and the newly formed proximal pink part of the nail appeared after abrupt cessation of smoking.
Smoking can also affect the tongue, palate and other anatomical structures of the oral cavity. In smokers, you can find characteristic hyperplasia of the papillae and black pigmentation of the dorsal surface of the tongue, the so-called. "black hairy" tongue. Smoker's tongue (or nicotine leukoplakia of the tongue, leukokeratosis nicotina glossi) is a homogeneous keratosis with inflamed salivary glands that look like papules with a depression in the middle. Smokers of bidis (tobacco wrapped in Cromandel ebony leaf) experience central atrophy of the tongue papillae, which is reversible upon cessation of smoking. Smoker's palate (or nicotine leukoplakia palati, leukokeratosis nicotina palati) is an asymptomatic homogeneous keratosis of the posterior two-thirds of the hard palate associated with multiple red, centrally depressed papules representing inflamed salivary glands. This can only be found among smokers, especially among avid pipe lovers. On the other hand, tobacco chewers develop a white discoloration at the site of contact with the tobacco, which may ulcerate (Fig. 2)
Figure 2| Keratosis caused by chewing tobacco (smokeless tobacco keratosis)
Hyperkeratosis of varying severity developed at the site of contact of the mucous membrane with tobacco. Grade 1 (a) mucous membrane of normal color with slight superficial wrinkles. Wrinkles disappear when the mucous membrane is stretched. Grade 2 (b) a combination of white-gray and reddish areas with moderate wrinkles. When stretched, neither wrinkles nor color disappear. The different thickness of wrinkles of more severe grade 2 (c) is noteworthy. Grade 3 (d) is similar in color to the more severe grade 2 (white-gray and reddish), but the mucous membrane shows deep, thick wrinkles that do not disappear with tension. The longer the habit, the higher the degree. The patient in photo (d) has an area of ulceration at the top of the mucosal area in contact with tobacco. Quitting the habit, especially if it lasts for a short period of time, leads to regression of damage.
Premature aging of the skin One of the most characteristic and socially significant manifestations of smoking is premature aging. The “smoker’s face” is typically mottled with pronounced wrinkles, facial features become thinner, emphasizing the bone relief, the skin is atrophic with a grayish tint against the background of plethora [10]. The degree of change is directly related to the number of cigarettes smoked per day (Fig. 3). Premature aging is more pronounced in women than in men. The severity of wrinkles is enhanced by direct contact with cigarette smoke, which dries out the stratum corneum of the epidermis and causes a moderate inflammatory reaction [12]. In vivo experiments in mice also show that passive exposure to tobacco smoke leads to premature skin aging [13]. Skin that is exposed to tobacco smoke is thin and fragile and tends to sag. While tobacco smoking itself is an independent risk factor for wrinkle formation, exposure to sunlight enhances this effect [14]. Smoking also affects skin that is protected from the sun. The best predictors of aging are the number of cigarettes smoked per day and age.
Figure 3 | Manifestations of smoking on the face of a smoking twin
Noteworthy are the significant differences in the appearance of smoking twin 1 compared to non-smoking twin 2. Twin 1, according to anamnesis, has about 52.5 pack/years (the number of packs of cigarettes smoked per day multiplied by the total duration of smoking in years). The total lifetime insolation of twins is comparable.
Cigarette smoke is an important factor in accelerating the aging process due to the formation of free radicals and the development of corresponding pathological processes (Fig. 4). Smoking can wear down cellular defense and repair mechanisms, leading to the accumulation of damage associated with mutations and defective proteins. Smoking also disrupts the renewal of intercellular substance in the skin [17], which leads to an imbalance between the processes of synthesis and degradation of proteins in the connective tissue of the dermis. In addition to the fact that smoking reduces the synthesis of collagen types I and III (an important condition for accelerated skin aging) [18], it also increases the content of tropoelastin and accelerates collagen degradation [19]. Smoking is an independent risk factor for an increase in the number of elastic fibers of the papillary dermis in skin not exposed to direct contact. This increase is a consequence of increasing degradation of the elastic substance, similar to solar elastosis [20]. Disturbances in the intercellular substance of connective tissue may contribute to the molecular mechanisms of premature skin aging in smokers. In vitro experiments show that collagen biosynthesis in cultured fibroblasts is significantly reduced after exposure to tobacco smoke extract [18]. Smoking increases the expression of matrix metalloproteinases (MMP-1, MMP-2, MMP-3, MMP-7, and MMP-8) [17,19]. In the skin of smokers, compared to non-smokers, the expression of MMP-8 is increased, and the expression of TIMP-1, an MMP inhibitor, is decreased. Increased expression of MMP-1 in active smokers is also detected in areas of the skin protected from the sun. In vitro experiments have shown that tobacco smoke extract can enhance the expression of MMP-1 and MMP-3 in dermal fibroblasts. Moreover, MMP-1 expression is significantly increased in fibroblasts after stimulation with tobacco smoke extract and UVA1 ultraviolet irradiation, independently of each other [18].
Figure 4 | The mechanism of premature aging caused by smoking
Smoking increases the amount of ROS and MMPs, which leads to collagen degradation and disruption of the structural integrity of the extracellular matrix. This reduced mechanical pressure on fibroblasts leads to an increase in intracellular oxidant levels - this, in turn, stimulates MMP-1 expression even more. FB - fibroblasts; ROS - reactive oxygen species.
Transforming growth factor (TGF)-b1 likely plays a role in age-related skin changes associated with tobacco smoking. Tobacco blocks the cell response to TGF-b by negatively regulating the TGF-b1 receptor and inducing non-functional forms, suggesting a role for TGF-b1 modulation as a possible way to inhibit premature skin aging [22]. Nicotine may impair dermal remodeling by increasing the activity of cell cycle regulators, apoptosis, and the amount of collagen Ia1, elastin, and MMP-1 [23]. By changing the metabolism of intercellular substances and nAChR expression, it can influence physiological aging. Nicotine also promotes elastin overproduction and keratinocyte nAChR-α7 overexpression. However, the nicotinergic effect on dermal fibroblasts is mainly mediated by the nAChR-a3 subtype [24]. Skin cancer Epidemiological studies have identified both positive and negative relationships between smoking and the incidence and aggressiveness of certain types of skin cancer. The development of smoking-induced skin cancer is explained by the following mechanisms: accelerated aging, mutagenesis, stimulation of tumor cell growth and invasion, neovascularization and stromal remodeling. Despite the fact that there are studies that did not find any relationship with smoking, [25] most studies have found that smoking is an independent risk factor for the development of squamous cell carcinoma (SC), in particular, SC of the penis, vulva, cervix and anus [ 26]. Quitting smoking reduces these risks [27]. Smoking increases the incidence of highly aggressive forms of vulvar PR and reduces survival. Women who smoke and have genital warts are 35 times more likely to develop vulvar cancer, suggesting a synergy between smoking and genital warts [27]. A significant relationship between malignant neoplasms of the oral cavity and smoking has also been established [28]. Smoking unfiltered cigarettes further increases the risk [29]. Women who smoke are particularly susceptible to oral malignancies [30]. Most studies have not found a clear association between smoking and the risk of basal cell carcinoma (BCC) [26], but the data are conflicting. Cigarette smoking may be associated with a predominance of larger BCCs (>1 cm in diameter) [31] and more aggressive forms [32]. Earlier studies that examined the relationship between smoking and melanoma found that the number of men who smoked was in remission five years after diagnosis was significantly lower than that of non-smokers [33]. Smokers are more likely to have early and visceral metastasis [34]. More recent studies, however, show that smoking habit has no effect on the risk of malignant melanoma [26]. Long-term smoking may even reduce the risk of developing melanoma, especially acral melanoma [35]. The protective effect of smoking on cutaneous melanoma may be associated with the participation of nicotine in melanin synthesis, its affinity for melanin-containing tissues, irreversible binding to melanin, and the deposition of tobacco carcinogens NNK and NNN in tissues containing melanin. It is noteworthy that using the example of hairless mice, the inhibitory effect of tobacco components, caused by a block of the nuclear factor-jB signaling pathway, on skin tumors induced by UVB irradiation was demonstrated [13]. Smoking is associated with a reduced risk of classical Kaposi's sarcoma (cKS) [36] and AIDS-associated Kaposi's sarcoma. However, in clinical trials, transdermal nicotine in the treatment of KS in non-smokers was ineffective against KS lesions or HHV-8 viral load [38]. The carcinogenicity of tobacco is mainly associated with the action of PAHs, nitrosamines and heterocyclic amines. It is known that smoking slows down the repair of single-stranded DNA breaks [39] and also has a direct oncogenic effect [40]. The pro-tumorigenic effect of nicotine is also explained by an increase in the frequency of mitosis of cells in the basal layer and the appearance of hypertrophied epithelial cells in the epidermis [41]. Nicotine and nitrosamine contained in tobacco promote tumor growth through the positive regulation of cellular nAChRs, which induces the invasion of malignant cells and inhibits apoptosis [42]. The proinvasive effects of nicotine are due to nAChR-α7 [43]. Nicotine increases the secretion of acetylcholine, as well as the expression and activity of nAChRs in malignant cells [44]. Receptor-mediated toxicity of tobacco is the result of the interaction of the downstream signaling pathways Ras/Raf-1/MEK1/ERK, as well as JAK-2/STAT-3, starting with the activation of nAChR-α7 keratinocytes (Fig. 5) [45]. Nicotine has also been shown to stimulate tumor growth by increasing the activity of phospho-ERK (phosphorylated extracellular signal-regulated kinase). The proliferative effects of nicotine can be prevented by using a high-affinity nAChR-α7 blocker, α-cobratoxin [46]. Pharmacological block of nAChR-α7 disinhibits apoptosis and reduces the expression of vascular endothelial growth factor (VEGF), which leads to inhibition of angiogenesis [47].
Figure 5 | Interaction of the downstream signaling pathways Ras/Raf/MEK/ERK and JAK-2/STAT-3 with nAChR-α7 of keratinocytes
Stimulation of nAChR-α7 by both the physiological ligand acetylcholine and nicotine leads to changes in gene expression through transactivation of STAT-3. Transactivation can occur through two signaling pathways associated with nAChR-α7. The pathway of sequential activation of Ras/Raf/MEK/ERK leads to an increase in the concentration of STAT-3 in the cytoplasm, due to the positive regulation of expression, while activation of the tyrosine kinase JAK-2 causes phosphorylation of STAT-3 with subsequent translocation of STAT-3 dimers into the nucleus, where there will be a change in gene expression.
Indirect oncogenic effects of nicotine associated with endothelial cells and fibroblasts of the dermis are also known. Nicotine can enhance tumor growth by enhancing tumor vascularization and creating a pro-carcinogenic environment in the stroma [49]. The effect of smokeless tobacco extract on dermal fibroblasts enhances the production of factors that accelerate the proliferation and germination of immortalized keratinocytes. Thus, ultraviolet light and nitrosamines from tobacco can induce carcinogenesis, while nicotine promotes the growth and proliferation of altered cells. Impaired wound healing Smokers have an increased risk of complications from surgical wounds [50]. Animal studies have shown that smoking within eight weeks before surgery increases the likelihood of skin flap necrosis [51]. At the same time, abstaining from smoking reduces the likelihood of infectious complications [52]. The pathobiological basis for changes in wound healing caused by tobacco are similar to those associated with premature skin aging. For example, collagen production is also reduced and intercellular metabolism is altered, with MMP-8 levels increasing. It has been shown that this contributes to disruption of regeneration processes. It is likely that smoking also affects wound healing by inhibiting the migration of fibroblasts to the wound bed, which leads to their accumulation at the wound edge. Increasing the lifespan of fibroblasts simultaneously with decreasing their migration may promote fibrosis and excessive scarring [54]. It is important that epithelization of the wound is caused by the migration of keratinocytes over the exposed dermis. Keratinocyte migration is regulated by both nicotinic and muscarinic subtypes of ChR. It can be inhibited by activation of nAChR-α7, which are responsible for coupling ion flows with cascades of protein kinase signaling pathways that regulate integrin expression and Rho kinase activity [55–58]. Smoking may slow wound healing indirectly through slowing blood flow. While smoking reduces blood flow, oxygen concentration, and aerobic metabolic activity in the skin, nicotine itself increases tissue oxygen content, even despite reduced blood flow [59]. Most likely, the effect of smoking on microcirculation is not due to the effects of nicotine. It is likely that nicotine affects regeneration only in toxic doses. In the therapeutic range, however, transdermal nicotine has been shown to be different: it normalizes microvascular perfusion of the digital skin [60] and stimulates wound healing and angiogenesis [61]. In an experiment on mice, nicotine significantly promoted regeneration [62]. In addition to the positive regulation of the rate of epithelialization, the mechanism is probably associated with increased synthesis of type I collagen [63]. Chronic dermatoses affected by smoking Contact dermatitis Cigarette smoking and snuff use are proven risk factors for the development of allergic contact dermatitis. The following allergens are found in cigarettes: cocoa, menthol, licorice, rosin and formaldehyde [64]. Smoking dose-dependently increases the likelihood of a positive skin test for nickel [65]. Nicotine, itself an allergen, in skin tests can cause allergic or simple contact dermatitis at the site of application [66]. Atopic dermatitis Although smokers have significantly higher serum IgE titers than nonsmokers, evidence regarding the effect of smoking on atopic dermatitis is inconsistent. Some studies report that smoking is an independent risk factor for hand eczema [68]. However, other studies have not found such a relationship between smoking and atopic dermatitis or hand eczema [69]. Psoriasis A significant direct correlation between psoriasis and smoking, depending on the number of cigarettes smoked per day, is well known [69]. Smoking is an independent risk factor for psoriasis [70], more dangerous in men [71]. Moreover, periods of remission after treatment are shorter in smokers [72]. Palmoplantar pustulosis (PPP) PPPP (Figure 6) is one of the most common inflammatory skin diseases associated with smoking. About 95% of all patients with DILI are smokers, the majority are heavy smokers [73]. Quitting smoking significantly improves the condition: fewer pustules, less area of erythema with scaling [74]. The target of inflammation in DILI is the acrosyringium (Intraepidermal part of the sweat gland duct - editor's note). Due to impaired expression of nAChRs and other components of the skin cholinergic system, patients with DILI may develop an abnormal inflammatory response to nicotine. These observations indicate a role for nicotine in the pathogenesis of DILI [75].
Figure 6 | DILI, also known as “pustular psoriasis”
Cutaneous lupus erythematosus Studies have found a statistically significant association between active smoking and the development of cutaneous lupus erythematosus [76]. An association between discoid lupus erythematosus (DLE) and smoking has also been shown. Smokers with DLE have more extensive lesions at disease onset [77]. Also, the effectiveness of antimalarial drug therapy is reduced by smoking [78]. Hair and hair follicle diseases Smoking is associated with premature graying of hair in both men and women, as well as earlier hair loss in men [79]. The course of androgenetic alopecia is aggravated by frequent smoking, and the onset occurs earlier, the higher the dose [80]. In vivo studies have shown that in mice exposed to tobacco, epidermal atrophy develops, subcutaneous fat tissue becomes thinner, and the number of hair follicles decreases. Cellular apoptosis is also observed in the hair follicle [81]. Smoking affects the microvasculature of the hair papilla in the dermis and leads to DNA damage in hair follicle cells [82]. It also unbalances the protease-antiprotease system, leading to changes in the hair growth cycle. An increase in the concentration of proinflammatory cytokines causes microinflammation and fibrosis of the follicles. Pustular dermatoses While some studies suggest a dose-dependent linear relationship between the incidence and severity of acne vulgaris and tobacco smoking [83], other studies have not revealed such a relationship [84]. In contrast, a lower prevalence of acne has been reported among smokers [85]. The risk of developing rosacea is also lower among smokers, probably due to the vasoconstrictive effects of smoking [86]. A clear relationship has been established between smoking and hidradenitis suppurativa (the so-called acne inversus) [87]. The key element in the pathogenesis of hidradenitis suppurativa is probably choline-sensitive cells of non-nervous origin, as evidenced by the abnormal expression of nAChRs in the skin involved [88]. Pemphigus vulgaris It is noted in the literature that pemphigus vulgaris develops more favorably when smoking. This is consistent with data that among patients with pemphigus, smokers make up a minority [89]. Smokers with pemphigus vulgaris go into partial and complete remission more often than non-smokers [90]. There is also an inverse relationship between tobacco smoking and dermatitis herpetiformis and associated celiac disease [91]. Smokers with newly diagnosed celiac disease are less likely to have endomysial antibodies than nonsmokers [92]. However, one study did not find any association between smoking and the presence of antigliadin antibodies [93]. No significant relationship was found between smoking and mucosal pemphigoid [94]. Skin ulcers Smoking is a risk factor for the development of pressure ulcers [95] and infected ulcers in patients with diabetes [96]. More than 90% of patients with ulcerative lesions due to Buerger's disease (thromboangiitis obliterans) are smokers. Long-term remissions are possible when smoking is stopped, while relapses are caused by a return to the bad habit [97]. Viral skin diseases Smoking is known to increase the risk of genital warts in men [98]. But the incidence of recurrent herpes labialis in smokers, on the contrary, is much lower, especially when smoking a pipe [99]. This is most likely due to the ability of tobacco to inhibit the replication of the herpes simplex virus and significantly reduce its cytolytic effect [100]. However, more recent studies have shown that nicotine applications via a transdermal patch induce herpes simplex virus reactivation as well as viral shedding in rabbits carrying the infection [101]. Other diseases of the skin and mucous membranes A significant association has been established between smoking and diabetic necrobiosis lipoidica [102]. Smoking has also been associated with generalized urticaria [103]. Men who smoke cigarettes or beedis are at significantly higher risk of developing arsenic-related skin lesions than non-smokers [104]. On the other hand, there is an inverse relationship between tobacco smoking and geographic language [105]. Skin diseases treated with nicotine As noted above, smoking can aggravate the course of certain diseases, promote carcinogenesis and potentially lead to addiction. However, no matter how paradoxical it may be, in the case of many dermatological diseases, nicotine shows itself to be an effective monotherapy. Buerger's disease is clearly associated with smoking but is successfully treated with nicotine-containing chewing gum (Fig. 7) [106]. It is likely that other components of tobacco induce vasospasm and aggravate thromboangiitis obliterans, but the use of nicotine may have valuable therapeutic potential. In addition, a key component of treatment for Buerger's disease is smoking cessation.
Figure 7 |Buerger's disease during nicotine treatment
(a) Left big toe with a large deep ulcer (1.5–2.0 cm) in a 38-year-old man who has been smoking for 20 years. (b) The ulcer healed 20 days after starting treatment with nicotine chewing gum (2 mg per piece) given twice daily. At least 14 months later, while taking 2 nicotine gums per day without other medications, the patient's legs remained in good condition, with no ulcers or intermittent claudication.
The therapeutic effect of cigarette smoking on aphthous ulcers of the oral and genital mucosa in Behçet's disease is also known [107]. Accordingly, cessation of smoking leads to the appearance of mucocutaneous manifestations, especially aphthous stomatitis. However, when treated with nicotine, aphthous ulcers resolve within a few days [108]. The mechanism of this action is likely related to the ability of nicotine to inhibit the release of proinflammatory cytokines IL-6 and IL-8 from keratinocytes and endothelial cells in the dermis. Tobacco smoke extract also reduces IL-8 release but increases VEGF production in human keratinocytes [109]. Inflammatory bowel diseases (IBD), according to epidemiologists, are associated with smoking [110]. Smoking and/or consumption of pure nicotine can affect such mucosal and skin manifestations of IBD as aphthous stomatitis, pyoderma gangrenosum and erythema nodosum. Most patients with ulcerative colitis are nonsmokers or have stopped smoking [111]. Smoking cessation worsens the progression of ulcerative colitis (UC), but progression slows again when smoking resumes. In contrast, patients with Crohn's disease who smoke tend to have a more severe course [112]. Nicotine is a key component of tobacco that has an effect on IBD, as its administration through transdermal patches is known to inhibit inflammation in UC, which is not observed in Crohn's disease [113]. Interestingly, mice with trinitrobenzene sulfonic acid-induced colitis that received the nAChR-α7 agonist anabasine had less tissue damage than mice that did not receive it [114]. Nicotine has also been used in the treatment of pyoderma gangrenosum and erythema nodosum, probably associated with IBD, and in the treatment of malignant atrophic papulosis (so-called Degos disease) [117], Kimura disease [116] and eosinophilic pustular folliculitis [118]. Similar to ulcerative colitis, recurrent aphthous stomatitis (RAS) is less common in smokers [119]. It is known that aphthous stomatitis also suddenly worsens with a sudden cessation of smoking, and weakens when resumed. Nicotine replacement therapy significantly reduces the relapse rate of ASD, suggesting that nicotine could be used as a drug [120]. Although published studies do not suggest an association between smoking and lichen planus (LP) of the oral mucosa, there is one case of otherwise resistant LP that responded to nicotine gum [121]. Transdermal nicotine has been shown to directly reduce inflammation in the skin [122]. Nicotine and other nAChR agonists may exert anti-inflammatory effects by inhibiting lymphocyte proliferation, endocytosis and phagocytosis by dendritic cells, as well as the production of ROS, superoxide and pro-inflammatory cytokines [123]. It is likely that the mechanism of anti-inflammatory action is also due to anti-inflammatory cytokines, IL-10 and TGF-b, glucocorticoids and soluble receptors that neutralize the effects of pro-inflammatory cytokines. Nicotine stimulates nAChR-α7, which modulate inflammation in the absence of parasympathetic innervation. This is an essential receptor necessary for the inhibition of cytokine synthesis during the implementation of cholinergic anti-inflammatory pathways [124]. On the contrary, the absence of nAChR-α7 leads to an increase in the pro-inflammatory cytokine response [125]. Conclusion Tobacco and its components affect the skin directly and indirectly. Various skin cells express nAChR subtypes, the activity of which influences cell viability and function. Changes in the skin are caused by both genomic and non-genomic effects of tobacco toxins and nAChR agonists. The effects are varied: from accelerating the aging process to mutagenesis. Epidemiological studies have established both positive and negative relationships between tobacco smoking and various skin diseases. A positive relationship with certain diseases may have a beneficial effect on their course upon smoking cessation, while the opposite may require specific treatment with nicotine agonists. It is important to understand the difference between the effects of tobacco and pure nicotine in Buerger's disease. Part of the anti-inflammatory effect of nicotine is due to stimulation of nAChR-α7. The effects of tobacco components and pure nicotine are summarized in Table 1. Further research is needed on nicotinergic substances as potential therapeutic agents for certain skin diseases. Table 1 | Generalized effects of tobacco/nicotine on skin