Regurgitation is the reflux of a small amount of gastric contents or gastric juice mixed with saliva up the esophagus. Regurgitation often occurs in infants and in the vast majority of cases is a variant of the physiological norm. They do not require therapy except in a few cases, which will be described below.
The younger the child is, the more often he can regurgitate. As the child grows, they gradually disappear until they disappear completely. In the first month, regurgitation occurs in 85% of children; this indicator does not depend on the type of feeding (formula or breast milk) and on the method of administration (bottle or natural feeding). After 3 months, regurgitation occurs much less frequently, and by one year it disappears completely.
At CELT you can consult a pediatrician.
- Initial consultation of a patient under the age of 17 inclusive - 2,500
Make an appointment
Causes and mechanism of regurgitation
The following reasons are identified:
- Filling the stomach with air, which the child can swallow while eating. This is the most common reason, which requires practically no special correction.
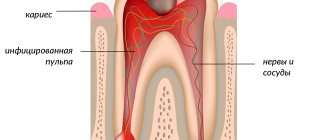
- Muscular weakness of the valve between the esophagus and stomach. It develops as the child grows and begins to function normally by the first year of life. Therefore, food can pass from the stomach into the esophagus without hindrance, which is what happens during regurgitation.
- Food allergies (or food intolerances). Most often it manifests itself as skin reactions, but in rare cases, regurgitation may be a symptom.
- Congenital defects of the gastrointestinal tract. The digestive system is quite complex; some disturbances in its structure can lead to digestive problems that begin to appear immediately after birth. Thus, narrowing in the area of the gastrointestinal junction can lead to frequent atypical regurgitation.
Next, we will provide recommendations on how to distinguish pathology from the norm, and when you need to see a doctor. If regurgitation is caused by a disease, then it is reasonable to begin treatment as soon as possible.
What is hypersalivation?
Increased salivation can be attributed to natural physiological processes between the ages of 2 and 8 months.
Intensive production of excessive amounts of secretion by the salivary glands is called hypersalivation.
The etiology of ptyalism can be pathological or physiological. In newborns, due to underdevelopment of the salivary glands, there is no salivation.
Increased salivation can be attributed to natural physiological processes between the ages of 2 and 8 months.
If signs of hypersalivation appear at an older age, then this indicates the presence of pathological processes in the body.
In medical practice, the following types of hypersalivation are distinguished:
- True. Associated with increased secretion of the salivary glands. Depending on the etiology, it can be bulbar, somatic, medicinal and psychogenic.
- False. Caused by dysfunction of the physiological process of swallowing saliva.
Important! With a severe degree of development of ptyalism, the integrity of the skin may be damaged under the influence of the constituent components of saliva.
Regurgitation and vomiting
Regurgitation is in most cases a physiological phenomenon that does not require special treatment or observation. But it may look like vomiting, being a sign of dangerous diseases, in which case consultation with a doctor is necessary. Regurgitation and vomiting have a similar mechanism of occurrence, namely, the release of gastric contents into the oral cavity.
It is important to distinguish between them, since vomiting in newborns is very dangerous and can lead to aspiration of contents into the respiratory tract and respiratory arrest.
There are differences between regurgitation and vomiting:
- Regurgitation most often occurs after eating. Usually this is a single, non-repeating episode. The child regurgitates the food he has just eaten; there are no foreign impurities in it.
- Vomiting usually occurs repeatedly. It happens not related to food intake.
- Regurgitation does not affect the child’s well-being and mood - he is active, does not show signs of anxiety, smiles, and plays.
- Vomiting is accompanied by a deterioration in general health. The child is lethargic or restless.
- Regurgitation usually occurs suddenly, and vomiting is preceded by a decrease in activity and mood.
- Vomiting is rarely the only symptom; other problems with the functioning of the digestive tract or fever are also observed.
Vomiting in a child is a reason to see a doctor!
Whooping cough in children: from infants to adolescents
Whooping cough is one of the most serious and long-lasting infections, which is especially dangerous for children in the first year of life, and today there are cases of its development even in babies 2-3 months old.
The disease is severe, lasting up to 10 weeks or more, characterized by bouts of painful coughing that cannot be relieved by medications.
Today is the day whooping cough is no longer a rare infection. In 2022, according to Rosstat, children began to get whooping cough 2.3 times more often than in the previous year.
Over the past ten years, the incidence has been steadily increasing. And most of the patients are young children, children of the first three years and preschoolers, that is, those for whom the disease is most severe.
This increase in incidence is due to the fact that children are increasingly not given the DTP vaccine or do not receive a full course of vaccinations in the 1st–2nd year of life.
And almost none of the parents care about additionally vaccinating their children against whooping cough before going to school.
Whooping cough: what do we know about it?
Although cough is accompanied by many childhood diseases, whooping cough is special: 10–40 attacks of dry hacking cough per day exhaust both the child and the parents.
Episodes of coughing last from a few seconds to 2–3 minutes and lead to choking and vomiting. Coughing attacks end with a loud, high-pitched “cock crow.” This is the sound of a child frantically trying to breathe in air between repeated coughing attacks.
Repeated episodes of painful coughing are called “paroxysms,” which gives the condition another name called “paroxysmal cough.” Doctors themselves sometimes call whooping cough the “100-day cough,” which is due to its duration, which is about 6–8 weeks, and the intensity of the attacks gradually decreases.
No matter how painful and dangerous it can be, whooping cough, when diagnosed early, is treatable and can be prevented with a vaccine.
But in order to suspect whooping cough based on the first signs, you need to know that the child has been in contact with the patient and confirm the disease with test data - and this is not always easy.
Whooping cough is caused by the microbe Bordetella pertussis. They penetrate with particles of mucus, saliva and sputum when a sick child or adult sneezes or coughs into the mouth, throat and bronchi.
Bacteria penetrate the mucous membranes of the respiratory system, bind there to epithelial cells, and begin to produce cytotoxin, a special substance that affects the cilia of the ciliated epithelium that covers the respiratory tract. They help keep the airways clean, like a brush, clearing mucus and debris from the airways.
Cytoxin blocks their motor activity, and the child is forced to cough heavily, since the epithelium of the respiratory tract sends continuous signals that cleaning is needed. This leads to episodes of whooping cough.
Children can develop whooping cough if they are in close contact with infected adults or other babies. Bacteria are scattered a meter around the patient when he coughs or sneezes. Up to 80% of children become infected if they have not been vaccinated and have no immunity to this disease.
Is everyone at risk of getting sick?
Although the risk of infection in childhood is high, there are some conditions that significantly increase the likelihood of infection:
- Age less than 6 months. Infants are particularly susceptible to infection, especially if born prematurely. They do not yet produce an adequate amount of antibodies to protect themselves from dangerous microbes, so they must be protected from infections in every possible way.
- Children with weakened immune systems. Babies with congenital immunodeficiency or one of the forms of oncological pathologies are at greater risk than others of getting sick and having a hard time with whooping cough.
- Not immunized children. Babies who have not been vaccinated against whooping cough are also at great risk. During outbreaks, they may even be temporarily isolated from other babies.
Main signs of whooping cough
It is not easy to recognize an infection at the very beginning; it can begin like a normal ARVI, and only then do typical manifestations appear. On average, typical cough recurrences appear by the third or fourth week of infection. Symptoms occur in stages; there are several stages in the development of the disease:
First stage (first-second week). The leading signs of whooping cough in children are not pronounced: coughing with occasional sneezing is possible. If a cough does occur, it is quite normal; it does not yet resemble attacks of whooping cough. There may be a low fever, not reaching values more than 37.7 ° C.
Child behavior
The mechanism of regurgitation is such that components of gastric juice enter the esophagus along with the food eaten. As you know, it has high acidity and irritates the esophageal mucosa. As a result, the child experiences discomfort and can become quite restless. It’s very easy to check whether your baby’s anxiety is related to regurgitation - just lay him on his back. If the problem is regurgitation, then the baby will behave even more restlessly. If not, then the horizontal position will not bring him discomfort.
If regurgitation occurs frequently, it is called regurgitation syndrome. It can lead to complications - chronic irritation of the respiratory tract. As a result of the constant aggressive effect of gastric juice on the mucous membranes of the upper respiratory tract, the latter are susceptible to an inflammatory process. Therefore, it is important to monitor the child’s condition and, if necessary, consult a doctor.
How many times can there be a chair?
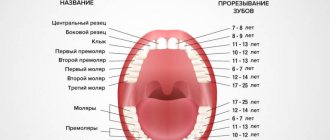
Diarrhea is also possible when teething
Quantity is one of the most important indicators. At first, the child may defecate up to 10 times per day. This is common in babies less than 4 months old. But there is one condition: the baby must feel good, the weight gain must be constant.
If the baby is breastfed, stool may be rare. There's nothing wrong with that. Even if the baby walks “largely” once every few days and feels good, there is no need to worry. However, you need to pay attention to the consistency of the stool; it should remain soft.
If the feces are hard, this is already a violation of the norm, which means there are digestive disorders. Diet violations made by a nursing woman can lead to this. Mom needs to monitor her diet more carefully, then everything will return to normal.
Tips for parents
Let's figure out how to avoid possible dangers associated with regurgitation. The main thing that responsible parents need to know is that most often children burp while lying down. This position is dangerous due to aspiration (inhalation) of gastric contents.
Preventing aspiration is simple - just bring the baby upright or turn him on his side or stomach immediately after he burps. Then the baby will be able to push food out of his mouth.
It is worth remembering that it is unacceptable to leave a child with regurgitation syndrome without adult supervision, especially when lying on his back.
What is it and how often does it happen
An intestinal infection is a disease that develops when viruses or bacteria enter the body and is manifested by diarrhea, vomiting, fever, weakness and dehydration.
According to WHO data for 2022, rotavirus infection accounted for 60% of cases of severe diarrhea in children under 5 years of age, and most of them were under one year of age. When the first symptoms appear in young children, it is necessary to seek medical help - up to 200 thousand children still die from rotavirus infection every year in the world, especially in developing countries.
Feeding rules
Frequent regurgitation can be prevented by following a few feeding rules.
- After feeding, it is necessary to hold the baby upright. Even if your baby is tired or wants to sleep, you shouldn’t put him to bed right away. It is very comfortable to hold infants on your shoulder. After waiting for the air to burp, the child can be given any position.
- The same should be done before feeding. The thing is that in an upright position the child can release excess air from the stomach. If this is not done before eating, belching is guaranteed.
- There is a certain position recommended for breastfeeding. One of the main goals of correct positioning of a nursing mother and baby is to prevent regurgitation. The semi-vertical position of the baby with the head raised above the level of the body must be maintained during each feeding.
- Feedings should be frequent, but in small portions. Overfeeding is fraught not only with regurgitation, but also with other digestive problems.
- It is important not to feed your baby when he is crying or laughing, otherwise he will swallow excess air.
- If feeding is carried out using a bottle with a nipple, it is necessary to ensure that the hole in the nipple is not too large, and the position of the bottle is such that the nipple is always filled with mixture and not with air.
- You should refrain from active games in the first half hour after feeding.
Following these simple rules will help reduce the frequency of regurgitation.
How is the intensity of regurgitation determined?
A special five-point scale is used for assessment, where:
- 1 point - up to 5 regurgitations per day in a volume of up to 3 ml;
- 2 points - more than 5 regurgitations per day in a volume of over 3 ml;
- 3 points - the baby burps more than 5 times during the day up to 1/2 the volume of milk or formula (up to half of the feedings);
- 4 points - each feeding is accompanied by regurgitation of a small amount of formula or milk for half an hour or more;
- 5 points - at least half of the feedings end with regurgitation of from 1/2 to the entire volume of milk or formula.
Danger signs
Responsible parents should be aware of dangerous symptoms that require consultation with a doctor:
- The baby is very restless and often turns around and arches his back when burping or feeding. This symptom may indicate chronic irritation of the esophagus.
- Regurgitation is frequent, abundant, observed after each feeding.
- The child is showing signs of dehydration.
- Regurgitation that first appeared after the first half of the year.
- Prolonged regurgitation without improvement (the same frequency and the same volume of regurgitation in a child 1 year and older).
- Regurgitation is accompanied by an increase in temperature.
- The child does not gain weight or even loses it.
- You cannot independently determine whether your baby is spitting up or vomiting.
There are even more dangerous symptoms, when they appear, you need to call an ambulance:
- The child stopped breathing after burping.
- A bluish tint appears on the lips and face.
- After regurgitation, the child lost consciousness.
- Reflux (stomach contents) that is green or brown can be a sign of intestinal obstruction or stomach bleeding.
Aspiration is extremely dangerous in infants who are unable to clear food from their airways on their own. The only thing parents can do is call an ambulance. It is not recommended to try to help your child on your own.
What should “normal” stool look like?
In the first months, infants have loose stools - this is the norm!
In the first months of life, all babies have loose stools. This is considered normal. You should not react to the advice of “well-wishers” who claim that the chair should be decorated. Perhaps such people simply don’t remember how it should be or don’t know anything, but want to seem knowledgeable on this issue.
A newborn baby cannot have formed feces; in this case, he simply would not be able to perform an act of defecation. The child cannot yet sit or stand and receives only liquid food, so he should only have loose stools. The body cannot form normal feces for an adult, because solid food particles do not enter and formed feces simply have nowhere to come from.
Therefore, parents should be calm about loose stools, which in adults is considered a deviation from the norm. There is nothing wrong with this for babies. But if the baby has hard feces, constipation will begin, which you will have to fight with your own means. After all, delayed bowel movements cause no less problems than diarrhea.
Parents need to monitor the consistency and color of stool; these indicators may change with age. Moreover, changes can occur every day. Such mobility of indicators is more common in breastfed children. Mom's diet will have a noticeable effect on the color of her stool. Therefore, even if an unfamiliar color appears, there is no need to panic; you must first analyze what the nursing woman ate. Standard indicators are given below.
Treatment
Treatment is required if respiratory complications occur or if irritation of the esophageal mucosa is suspected. In this case, the specialist will prescribe medications that reduce the acidity of gastric contents. This will not help with regurgitation, but will prevent further trauma to the esophagus. Specific medications are selected individually at an appointment with a pediatrician.
If the cause of regurgitation is an anatomical defect, surgical treatment may be required. Indications for surgery and its scope are specified by the surgeon.
For advice on infant feeding, please contact the specialists at the CELT clinic. Extensive experience, highly qualified clinic doctors and modern equipment are the key to the health and successful development of your children.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
How to get rid of this?
First of all, you need to determine the causes of excessive salivation. If it is pathological, then you cannot do without the help of a doctor and drug treatment.
If increased salivation is a physiological process, then parents need to alleviate the baby’s condition and support him during the period of hypersalivation:
- The restoration of the baby’s health depends on quick and adequate treatment.
When pathological changes occur in the oral mucosa in a child, it is necessary to consult a specialist. The restoration of the baby’s health depends on quick and adequate treatment.
- To get rid of hypersalivation , the cause of which is stomatitis or gingivitis, dentists prescribe medications that destroy infectious agents and promote rapid regeneration.
- If there is a helminthic infestation or a somatic disease , the symptom of which is increased secretion of the salivary glands, the child should be taken to see a doctor, examined completely and treated with medications that normalize salivation.
- Natural remedies will help improve the condition of the little patient. For stomatitis, it is recommended to rinse the mouth with table salt solution or herbal infusions, and for gingivitis - with sea buckthorn oil.
- You can reduce the secretion of saliva by strengthening the immune forces of the child’s body. For this purpose, they protect children from emotional stress, often take them for walks on the street, give them healthy food enriched with vitamins, and develop them physically by participating in various sports sections.
- Always use a bib. Treat the skin of the face with nourishing creams, and if necessary, dry the skin on the chin with the addition of zinc.
- Using pacifiers will help the baby reflexively swallow saliva when it is released in abundance.
Important! Self-medication of hypersalivation in children is strictly prohibited. Only the help of a qualified specialist will help to correctly establish the etiology of the pathology, on the basis of which appropriate treatment is prescribed.