Excessive tooth mobility is a common symptom indicating the development of severe dental diseases.
Unfortunately, many patients underestimate the danger of this pathology and postpone visiting the doctor until the last minute, depriving themselves of the opportunity to receive timely dental care. Meanwhile, in the absence of treatment, tooth mobility progresses and becomes irreversible. It is for this reason that any delay in starting restorative therapy significantly reduces the chances of maintaining the integrity of the dentition.
Causes of tooth mobility
Depending on the causes of occurrence, there are two types of tooth mobility:
- pathological;
- physiological.
Physiological mobility
Physiological mobility is determined by the need to evenly distribute the load on the dentofacial apparatus during chewing food. The amplitude of tooth movement is so small that the displacement cannot be noticed without additional research. The only evidence of physiological mobility is the formation of small ground areas at the lateral contact points of the teeth.
Pathological mobility
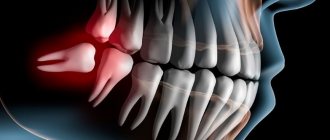
Pathological mobility is spoken of in cases where a change in the position of the teeth in the alveolar sockets becomes visually discernible. To describe the symptomatic picture of the pathology, the so-called Miller scale is used. The level of mobility is measured in points (from 0 to 3), with the upper value implying the ability of the tooth to move in all directions (including vertical).
Causes of pathological mobility
The causes of pathological tooth mobility can be:
- poor hygiene, the formation of an internal environment in the mouth that is favorable for the proliferation of pathogenic organisms, the appearance of soft and dense dental plaque;
- incorrect selection of individual hygiene products and devices, their illiterate use;
- pathological bite or unnatural position of individual teeth;
- endocrine disruptions in the body;
- untimely installation of prosthetic devices or implants after the loss of individual teeth;
- mistakes made by inexperienced dentists when providing certain dental services;
- anomalies in the structure of the dentofacial apparatus, too short frenulum of the tongue and lips;
- atrophy of the alveolar processes;
- inflammatory damage to the gum tissue, leading to dysfunction of the ligamentous apparatus of the teeth;
- injuries.
Signs of pathological mobility
Violation of the ligamentous apparatus, in which the tooth becomes loose, is accompanied by accompanying symptoms:
|
Classification of tooth mobility
In modern dental practice, to determine the degree of unnatural mobility of teeth, the classification developed by Honored Scientist of Russia David Abramovich Entin is most often used.
According to this typology, the following levels of mobility are distinguished:
- I degree (instability of position in relation to the coronal parts of adjacent teeth in the oral-vestibular or bucco-lingual directions, amplitude of movement less than 1 mm);
- II degree (mobility in similar directions with an amplitude of more than 1 mm, the appearance of movements in the distal-palatal direction);
- III degree (ability to move in all directions, including vertical);
- IV degree (adding rotational movements of the diseased tooth around its own axis).
What to do if an adult’s tooth is loose and hurts when pressed?
Normally, our teeth have little mobility. Dentists call it physiological; it is necessary to absorb the loads during chewing, as well as for their more even distribution over the entire dentition. But such mobility is so insignificant that it is impossible to notice it. Therefore, if an adult suddenly discovers that a tooth in his gum has begun to loosen, this is already a symptom or an indicator of pathology that requires the participation of a dentist. In the absence of timely medical care, such violations very often lead to irreversible loss of a tooth.
Treatment of unwanted tooth mobility
The treatment program for tooth mobility necessarily includes measures aimed at combating the underlying disease that provoked the development of the pathological process.
Otherwise, the scheme of therapeutic measures is individual in nature and can be supplemented by:
- carrying out professional hygienic treatment of teeth;
- selection of the most suitable individual hygiene products, devices for comprehensive dental care, teaching the patient the basics of their use;
- a set of measures aimed at eliminating malocclusion, the necessary orthodontic or surgical treatment;
- surgical or conservative treatment of periodontitis and other dental diseases.
If necessary, the doctor may decide to carry out a set of measures aimed at preventing further loosening of the teeth. Preference is given to splinting methods using removable and non-removable splinting structures.
The effectiveness of treatment depends directly on both the professionalism of the attending physician and the timeliness of therapeutic measures. That is why the detection of tooth mobility at any stage of the development of the pathological process is an absolute basis for contacting a doctor and receiving qualified dental care.
Treatment and strengthening of gums at the Family Dentist clinic
We have been treating gum inflammation since 2013, using low-traumatic tooth-preserving techniques.
Over the past 5 years, the clinic has provided assistance to more than 1,260 patients with periodontal diseases, completely eliminated or reduced the manifestations of inflammation, and restored damaged tissue.
The appointment is conducted by periodontist, associate professor Irina Leonidovna Bobkova, developer of a patented method of treating periodontitis with probiotic preparations in combination with low-intensity laser radiation.
Feedback from our patient
I thank Irina Leonidovna Bobkova for her clear, attentive attitude, professionalism and high-quality work.
10/30/19
Our dentistry takes a range of measures to preserve teeth:
|
|
If a tooth is loose, a periodontist will tell you how to strengthen the periodontal tissues. The doctor will select a comprehensive treatment that will strengthen the ligamentous apparatus and stop loosening.
Prevention measures
To prevent your teeth from becoming too loose, you need to maintain good oral hygiene. If you make it a habit to visit the dentist once every six months, the doctor will definitely tell you what measures will help strengthen your gums. The general rules are:
- ensure optimal load on the teeth - add hard vegetables and fruits to the diet;
- create a diet containing microelements and vitamins necessary for teeth;
- carry out professional cleaning of the oral cavity - remove stones and plaque.
In addition, regular consultation examinations will allow the doctor to detect the disease at an early stage.
Add a comment
Leave your comment
Diagnostics
Full recovery of the patient is possible only if a reliable cause of dentition instability is identified. The dentist conducts a full, comprehensive diagnosis for clients in order to develop an optimal treatment plan.
Advantages of our examination:
- Qualified personnel;
- Modern equipment;
- Using a complete list of examinations to identify the cause of the disease;
- Get results quickly.
Our doctors will be able to quickly understand the mechanism of the problem and immediately begin to treat it.
Selective grinding of teeth
- one of the most common methods in the system of complex therapy of periodontal diseases. According to some data, 95.8% of patients with periodontal pathology need it.
Objectives of selective teeth grinding:
1. Elimination of premature occlusal contacts
2. Elimination of moments that block and interfere with the movements of the lower jaw
3. Elimination of deformation of the occlusal surface of the dentition.
There are different methods of grinding teeth, the most popular are the Jenkelson and Schuller methods.
The technique proposed by Jankelson (1979) is considered a functional method, however, premature contacts are removed in central occlusion.
According to Jenkelson's classification, premature contacts are divided into 3 classes:
1st contacts on the vestibular slopes of the buccal cusps of molars and premolars and the vestibular surface of the lower incisors
2nd contacts on the oral slopes of the palatine cusps of the upper molars and premolars;
3rd contacts on the vestibular slopes of the palatal cusps of the upper molars and premolars.
Indications for selective grinding:
— Presence of premature contacts of antagonist teeth in central, anterior and lateral occlusions;
— Absence or uneven wear of hard dental tissues;
— Deformations of occlusal surfaces;
— Bite abnormalities
Method of selective grinding of teeth:
-carried out before therapeutic and surgical procedures or in parallel with them.
- Preliminary grinding of teeth involves shortening protruding teeth and is intended to eliminate significant deformations of the occlusal surfaces that occur due to defects in the dentition. If significant shortening is necessary, depulpation of the latter is indicated.
- The final sanding is carried out in a certain sequence. First, premature contacts in various types of occlusion are eliminated, then when moving the lower jaw from central to anterior and lateral occlusions.
- Before grinding, an occludogram is obtained, which is stored to monitor the results of grinding. After carrying out this manipulation, it is necessary to polish the ground surfaces and coat them with fluorine varnish.
Orthodontic preparation for orthopedic treatment for periodontal diseases
In patients with periodontal pathology, the clinical picture is often complicated by deformations of the dentition; in addition, malocclusions in some cases can themselves lead to periodontal pathology, so orthodontic preparation before orthopedic treatment is of great importance.
Structurally, orthodontic appliances have some differences from classical ones, these include:
— Application of minimal forces to move teeth.
- Longer active treatment and retention period.
Temporary splints can be used as retention devices.
Functional traumatic overload of the periodontium
-occupies a special place among local causes in the etiology and pathogenesis of periodontal diseases. When chewing and swallowing, at the moment of closure of the dentition, the periodontium of each tooth perceives a force load, which under normal conditions is absorbed by special periodontal devices (cemento-alveolar, interdental fibers, etc.). Then it is transformed and transmitted to the bone structures of the jaws, the temporomandibular joint and the skull. This physiological load helps normalize trophism and metabolism, stimulates the processes of growth and development.
With pathological processes in the periodontium caused by common causes (vitaminosis, diabetes and other disorders of endocrine regulation, diseases of the gastrointestinal tract, cardiovascular system and nervous systems, etc.), the resistance of periodontal tissues decreases.
As a result of weakening of the periodontium, the usual occlusal load begins to exceed the tolerance of its structures and turns from a factor stimulating development into a traumatic one, disrupting the trophism of the periodontium and destroying its tissues. Traumatic occlusion occurs, which subsequently plays a leading role in the course of this disease.
The term “traumatic occlusion” was proposed by PR Stillman in 1919. Other terms have been proposed to characterize and define periodontal overload:
- “traumatic articulation”
- “functional traumatism”
- “pathological occlusion”
- “functional traumatic overload of teeth”, etc.
According to the mechanism of development, three types of traumatic occlusion are distinguished:
— Primary
— Secondary
— Combined
Primary traumatic occlusion develops against the background of unaffected periodontium as a result of the action of an occlusal load that is excessive in magnitude and/or direction.
Thus, primary traumatic overload of healthy periodontium can occur due to excessive magnitude, abnormal direction and duration of action of the occlusal functional load and steam function of the masticatory, facial muscles and tongue. More often than not, overload is caused by the simultaneous action of several causes.
Secondary traumatic occlusion:
Its pathogenesis is based on pathological changes in periodontal tissue. At the same time, degenerative and inflammatory processes develop in the supporting tissues of the teeth throughout the entire dentition, which are accompanied by:
1). resorption of bone tissue of the alveolar process.
2). Gingivitis.
3). destruction of the periodontium with the formation of a pocket.
4). suppuration from it.
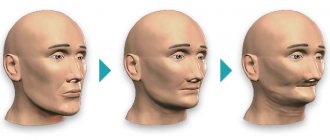
Resorption of the bone tissue of the sockets leads to a disruption of the normal biological patterns of the structure and function of the periodontium. From this moment on, a radical change occurs in the biomechanical relationship between teeth and surrounding tissues.
Thus, a change in the ratio of the extra- and inside the alveolar part of the tooth is one of the pathogenetic mechanisms in the development of traumatic occlusion.
The clinical picture of secondary traumatic occlusion is diverse and depends on the patient’s age, the form of the underlying disease (periodontal disease, periodontitis), its severity and stage of development, the presence of dentition defects, malocclusion or tooth position, pathological abrasion and other traumatic factors.
If for primary traumatic occlusion orthopedic intervention is sufficient, then for secondary occlusion complex therapeutic (local and general), surgical and orthopedic treatment is required. The prognosis also varies. In case of primary traumatic occlusion, after eliminating the overload of the teeth in all periodontal tissues, reparative processes occur.
Who is at risk?
Some chronic diseases in the body can also affect the strength of incisors and molars, including:
- cardiovascular diseases;
- arthrosis, arthritis, psoriasis;
- dysfunction of the thyroid gland.
Tooth mobility is typical in women during pregnancy, as well as in older people whose hormonal levels change and the body suffers from a lack of essential microelements.
Because of this, the gums become loose and can no longer securely hold the tooth in the socket. It is necessary to constantly monitor the condition of the soft tissues of the oral cavity and consult a dentist in a timely manner.