All people have a unique appearance and unique facial features. Some of us sometimes experience gaps between our teeth. Sometimes this defect may be subtle. But in other cases, such imperfection leads to serious physical as well as psychological consequences, and the issue of correcting this disorder is very relevant for a person.
Classification of dental gaps
Diastemas
– these are gaps of any size between the front central incisors. Tremae are spaces between any other teeth in the upper or lower jaw. Gaps between the lower front incisors are uncommon, but gaps between the upper central teeth can be seen several times more often. In many cases, the presence of a diastema of this kind provokes serious psychological discomfort, interfering with the harmonious socialization of patients.
Depending on what type of teeth are – baby or permanent – a distinction is made between false and true gaps between them. False dental gaps are observed in children - such defects go away on their own along with the change of teeth. True gaps form between permanent teeth and can only be removed with specialized help from a dentist. Doctors advise starting to correct such defects immediately after they occur, since then it will require much less time and effort.
Gap between teeth: what should be done?
If you have a very small diastema, then a visit to the dental clinic can wait. However, even a small gap should be regularly monitored by a doctor, since tooth gaps tend to grow over time. However, if the diastema is significant, it is better to visit the dentist as soon as possible. This defect can contribute to the development of caries, malocclusion, gum disease, etc. Various methods have been developed for correcting diastemas. Typically, the doctor carries out treatment on an individual basis and selects a method that will be most effective for a particular patient. The technique is chosen based on the reasons for the appearance of a gap between the teeth, the size and degree of development of the dental gap, and the wishes of the person himself.
Indications
Mobility of dental units is divided into three degrees of severity:
- There is mobility of up to 1 mm in the horizontal direction.
- Tooth mobility is more than 1 mm in the horizontal direction.
- The most complex degree with mobility of dental units in both horizontal and vertical directions.
In the first and second stages, there is a chance to save the tooth with the help of strengthening, for example, splinting. Removal of the moving wall in the third degree is inevitable.
Important! If you find even a small crack or chip on a tooth, you should not delay visiting the dentist. The smaller the defect, the greater the chance of restoring the tooth without removing it.
Use of artistic restoration
Some patients are advised to undergo aesthetic artistic dental restoration to eliminate diastema. This is a therapeutic intervention during which composite microprostheses (veneers) are installed on the two central incisors, between which there is a gap. The doctor uses a filling material that matches the patient’s natural enamel shade and builds up additional volume of hard tissue on the two central front teeth. To undergo this procedure, you only need to visit the clinic once.
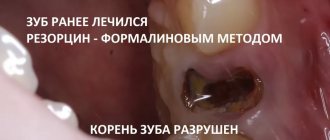
When restoring a tooth, the doctor restores its shape and function. The presence of colored deposits and cracks in the enamel, and other signs of destruction of dental tissue does not play any role, since most of the visible dental tissue is removed. Then its natural shape, color and functional properties are formed using composite materials (build-up method). If the root of a tooth is damaged, it is treated first, and restoration is carried out only at the next stage. If no pathologies associated with the tooth root are detected, then in 5-6 hours a qualified doctor is able to restore at least 4-5 teeth. However, if the dentist first works with the root of the tooth, then further manipulations are carried out after at least two days.
An important advantage of artistic restoration is its complete painlessness. Another important advantage of this method is its safety, therefore it has a minimal list of contraindications. Dental restoration can be performed on women even during pregnancy.
Surgical plastic surgery
For many patients, the determining factor in choosing a method for eliminating diastema is the cost of therapy. Be sure to consider your financial resources when you and your doctor select a method for correcting a dental gap. Choose the method that suits you best, but do not skimp on your health, as otherwise you may not achieve what you want and spend even more money on eliminating the negative consequences of unsuccessful treatment.
A tooth gap can also be removed using surgical plastic surgery. This technique involves installing dental crowns. Dentists correct the defect by placing ceramic veneers or crowns on the front teeth. This intervention allows you to achieve an excellent aesthetic effect that lasts for many years. Some disadvantage of this technique is its rather high price.
If for one reason or another you cannot use this technique, the doctor can fill the front teeth for corrective purposes, as a result of which the gap will be eliminated. Pay attention to the above method if the diastema occurs a second time or the installation of staples does not bring the desired result.
Orthodontic correction methods
Orthodontic methods for correcting diastemas are rightfully considered the safest, most effective and gentle (they allow you to preserve a maximum of healthy dental tissues). However, their main drawback is the long duration of treatment. Malocclusions are eliminated step by step - for this, braces are used. Orthopedic treatment is primarily indicated for children and adolescents whose permanent teeth have recently replaced their deciduous predecessors. Braces are special orthodontic structures that are attached to the teeth from the inside (invisibility braces) or the outside. How long do you need to wear braces? This is determined by the doctor individually, but usually treatment continues until the bite is completely corrected (from 6 to 24 months). It is best to install braces when the jaw is actively growing.
Your dentist may also recommend mouth guards, which are small transparent covers for your teeth. Aligners contain information about the normal shape and size of teeth. These devices are made in such a way that they move individual teeth in the required direction, restoring their correct position. The result of this is that the teeth move closer to each other and the diastema is eliminated. Aligners have a transparent base, so they are even less noticeable on the surface of the teeth than braces.
The advantage of mouth guards is that they can be removed while eating. Moreover, since they are filled inside with a whitening compound, using this method, you will not only eliminate the gap between the front incisors, but also lighten the tooth enamel. This will also add beauty to your smile and eliminate the need for additional whitening procedures.
Orthodontists are indispensable if a person, in addition to diastema, is diagnosed with any other malocclusion. Metal braces are considered affordable and reliable for most patients.
Text of the book “Fundamentals of clinical dental morphology: a textbook”
5.3.1.2. Age-related changes in the periodontium In the periodontium, throughout the life of an individual, plastic processes constantly occur in the renewal of its constituent elements: fibroblasts and other cells, collagen fibers and intercellular substance. The intensity of collagen renewal in the periodontium is 2 times higher than in the gums, and 4 times higher than in the skin. The high rate of collagen renewal is evidence of the important role of continuous periodontal restructuring in the constantly ongoing processes of adaptation of the supporting apparatus of the tooth to changing loads.
With age, the plastic capabilities of periodontal cells decrease, which is reflected in a decrease in the number of active cells (fibroblasts, osteoblasts, cementoblasts), a reduction in the synthesis of collagen fibers, and a deterioration in the blood supply to pericemental tissues. There is a decrease in the width of the periodontal fissure. These changes undoubtedly cause a weakening of the fixing apparatus of the tooth root, its barrier properties, and an increase in tooth mobility, which inevitably leads to the need for medical intervention.
5.3.2. Dental alveolus
Dental alveoli (alveoli dentales)
located in the alveolar process of the upper jaw and the alveolar part of the lower jaw. These sections of the jaws form as teeth develop and erupt and almost completely disappear with their loss.
Each alveolus is a bone socket in which a tooth is located. The edges of the alveoli do not reach the neck of the tooth (enamel-cement border), therefore the depth of the dental alveoli is slightly less than the length of the root of the corresponding tooth and the latter protrudes slightly from the jaw bones. This part of the tooth root is normally covered by the gum. The deepest is the canine alveolus. At the bottom of the alveoli there are usually several openings for blood vessels and nerves leading to the tooth.
In the alveolar process of the upper jaw there are 16 dental alveoli for the roots of the teeth. The alveoli are divided into vestibular (labial or buccal) and lingual (palatal) walls. The alveoli are separated from each other by bony interalveolar septa (septa interalveolaria). The alveoli of multi-rooted teeth also contain interradicular septa (septa interradicularia), which separate the roots of the tooth from each other.
The shape and size of the alveoli correspond to the shape and size of the tooth roots. The alveoli for the roots of the incisors are cone-shaped, with rounded outlines, the alveoli for the canine and small molars are oval and compressed in the mesial-distal direction. The alveolus of the first premolar of the maxilla is often divided by an interradicular septum into lingual and vestibular root chambers. The last three alveoli of the upper jaw, the largest in size, contain the roots of large molars. Each of them is divided by interradicular septa into three root chambers, two of which face the vestibular and the third face the palatal surface of the alveolar process.
The vestibular chambers are somewhat compressed laterally, so their size in the anteroposterior direction is smaller than in the palatobuccal direction.
The palatal (lingual) chambers of the alveoli have a rounded shape. Due to the variable number and shape of the roots of the third molar, its alveolus is variable in shape and can be single-chambered or divided into 2-3 or more parts.
The alveolar part of the mandible also contains 16 dental alveoli for the roots of the teeth, separated from each other by interalveolar septa. The walls of the alveoli facing the lips and cheeks are called vestibular, and the walls facing the tongue are called lingual.
The shape, size, and thickness of the walls of the alveoli are different for teeth of different groups. The alveoli of the incisors are compressed from the sides, and the thickness of the lingual wall of the alveoli is greater than the vestibular one.
The shape of the alveoli of the canine and especially the premolars is rounded, the lingual wall is also thicker than the vestibular one. The deepest is the alveolus of the canine and second premolar. The thickness of the walls here is greater than that of the alveoli of the incisors.
The alveoli of the molars contain interradicular septa: in the first two molars, one septum divides it into anterior and posterior chambers for the corresponding roots, and in the area of the third molar there may be one or more septa. Often the alveolus of this tooth is conical in shape without septa. The walls of the alveoli of the molars are thicker than those of the alveoli of the remaining teeth of the lower jaw.
In the alveolar process of the upper jaw and the alveolar part of the lower jaw, two parts are distinguished: the alveolar bone of the alveolar wall itself and the supporting alveolar bone. The first is a thin (0.1–0.3 mm) bone plate surrounding the tooth root, to which the fibers of the periodontal ligament are attached. It consists of lamellar bone tissue that forms osteons, is penetrated by a large number of perforating (Sharpey's) periodontal fibers and contains many holes through which blood and lymphatic vessels and nerves penetrate into the periodontal space.
The supporting alveolar bone includes:
- compact bone
forming the outer (buccal or labial) and inner (lingual or oral) walls of the alveolar process, also called cortical plates;
– spongy bone,
which is located between the walls of the alveoli and the cortical plates.
The cortical plates of the alveolar process, without a sharp border, pass into the bone of the jaw body. The thickness of the plates is not the same in different parts of the alveolar process and the alveolar part: they are much thinner in the upper jaw than in the lower jaw. They reach their greatest thickness in the area of premolars and molars of the lower jaw, as well as on the lingual side.
Spongy bone fills all the spaces between the walls of the dental alveoli and the cortical plates, and also forms interradicular and interdental septa.
The crossbars (trabeculae) of the cancellous bone distribute the forces acting on the walls of the alveoli to the cortical plates, so their location usually corresponds to the direction of the forces acting on the alveoli during chewing movements. Thus, in the area of the lateral walls of the alveoli they are located predominantly horizontally, and at their bottom they have a vertical course.
The spaces between the trabeculae of the cancellous bone are filled with red bone marrow in childhood and adolescence, and with yellow bone marrow in adults. Individual areas of red bone marrow may persist throughout life [67].
5.3.2.1. Age-related changes in the dental alveoli
During the life of an individual, the bone tissue of the wall of the dental alveolus, as well as the supporting bone of the alveolar process, is in a state of constant restructuring. this ensures adaptation of the alveolar bone tissue to changing functional loads, which is clearly manifested during physiological and orthodontic tooth movements.
With age, teeth gradually wear down on the occlusal and proximal surfaces. The abrasion of the tooth is compensated by its gradual advancement from the bone alveolus. Important mechanisms of this process are, first of all, the deposition of cement in the area of the root apex, as well as the restructuring of the alveolar wall, at the bottom of which and in the area of the interradicular septa, new bone tissue is formed.
When the approximal surfaces are worn away, the teeth become less convex, but the contact between them is not disrupted, since at the same time the interdental septa become thinner (Fig. 116).
Rice. 116. Restructuring of the walls of the dental alveoli with age.
1 – enamel; 2—dentin; 3 – interdental gum (papilla); 4 – walls of the bony alveoli.
This compensatory process is known as approximal, or medial, displacement of the teeth, the driving factors of which are occlusal forces, as well as transseptal periodontal fibers that bring the teeth together. In this case, a number of changes occur in the wall of the alveoli and periodontium, which can be designated as a physiological restructuring of the supporting apparatus of the tooth.
On the medial side of the alveoli (in the direction of tooth movement), narrowing of the periodontal space and bone resorption occur. On its lateral side, the periodontal space expands, the fibers of the pericementum are stretched, and on the wall of the alveoli, new formation and deposition of coarse-fiber bone tissue occurs, which is later replaced by lamellar tissue.
This ability of the alveolar bone tissue to restructure is widely used in orthodontic interventions aimed at moving a tooth to a new location.
At the same time, thanks to the use of special devices, it is possible to provide such an effect on the alveolar wall, which leads to resorption of bone tissue in the area of pressure and the formation of new bone tissue in the area of tension, i.e., to correction of the position of the tooth in the dentition in case of some anomalies of the dentofacial system . 5.3.3.
Desna Desna
is divided into three parts: attached, free and interdental (Fig. 117).
Rice. 117. Diagram of the structure of the gums.
I – gingival sulcus; 2 – gingival epithelium; 3 – free part of the gum; 4 – gingival groove; 5 – attached part of the gum; 6 – lamina propria of the gum mucosa; 7 – bone wall of the tooth alveolus; 8 – cement; 9 – periodontal ligament; 10 – attachment epithelium;
II – enamel.
Attached part
The gums are firmly fused with the periosteum of the alveolar process of the upper jaw and the alveolar part of the lower jaw.
Free part
Gums are the edge of the gum, which is loosely adjacent to the surface of the tooth crown, separated from it only by a narrow gap - the gingival sulcus. The gum does not have a strong connection with the periosteum and has some mobility. The border between the free and attached parts of the gum is a shallow groove - a gingival groove, located parallel to the gingival margin at a distance of 0.5–1.5 mm from it, approximately at the level of the bottom of the gingival groove or slightly above it.
Interdental part
forms a triangular interdental papilla, filling the gap between adjacent teeth. There are two types of interdental papillae - vestibular and lingual, connected to each other through the interpapillary ligament.
Due to constant mechanical stress during the process of chewing food, the epithelium and connective tissue of the gums have structural features of an adaptive nature. The gum is lined with multilayered flat, partially keratinized epithelium with an average thickness of 220–250 microns, which loses the stratum corneum in the area of the gingival sulcus (Fig. 118). The gingival surface covered by non-keratinizing epithelium is about 8-10%, keratinizing by orthokeratosis - 12-15%, by parakeratosis - 70-75%.
Rice. 118. The structure of the gingival epithelium.
1 – epithelium; 2 – basal (germ) layer; 3 – lamina propria of the gum mucosa.
The cells of the basal layer of the gum epithelium are characterized by high mitotic activity, so the rate of epithelial renewal here is higher than in other areas of the oral mucosa. The basal layer contains numerous melanocytes that produce melanin, which accumulates in significant quantities in epithelial cells, determining the pigmentation of the gums.
The border between the epithelium and the lamina propria of the mucous membrane has a scalloped character due to the introduction of high connective tissue papillae of the lamina propria into it.
The gingival epithelium is directly continuous with the sulcal epithelium and the attachment epithelium. The sulcal epithelium forms the lateral wall of the gingival sulcus. At the apex of the gingival papilla it passes into the gingival epithelium, and towards the neck of the tooth into the attachment epithelium.
Gingival sulcus
(sulcus gingivalis) - a narrow slit-like space between the tooth and the gum, extending from the edge of the free part of the gum to the attachment epithelium. The depth of the groove is from 0.5 to 3 mm, on average about 2 mm. An increase in the depth of the gingival sulcus with age of more than 3 mm turns it into a gingival pocket between the gingival margin and the surface of the tooth. The bottom of the gum pocket can reach the level of the cervical part of the tooth enamel.
The gingival sulcus contains fluid in which there are desquamated epithelial cells, bacteria, and granular leukocytes that have migrated into the sulcus through the epithelium. Electrolytes, immunoglobulins, and antibacterial substances are transported from the blood into the gingival fluid.
Chemical analysis showed the presence of amino acids, peptides, carbohydrates, urea, bacterial toxins, enzymes (lysozyme, lactoperoxidase), and antibodies in the gingival fluid. Some antibiotics (in particular, the tetracycline series) can accumulate here in concentrations 4–8 times higher than their level in the blood serum. The volume of gingival fluid under physiological conditions is negligible, but it increases sharply during inflammation.
The epithelium of the sulcus is similar to the epithelium of the gums, but is thinner and does not undergo keratinization. Epithelial cells are small in size and contain a significant amount of tonofilaments in the cytoplasm. The border between the epithelium and the lamina propria of the mucous membrane is smooth due to the absence of connective tissue papillae. In the epithelium and underlying connective tissue there is a significant number of granular leukocytes, macrophages and lymphocytes.
The attachment epithelium is a continuation of the sulcus epithelium, lining its bottom and forming a cuff around the tooth, which is firmly connected to the enamel surface covered with the primary cuticle. In structure, it is a multilayered squamous epithelium, the thickness of which is greatest in the area of the bottom of the gingival sulcus (15–30 layers of cells) and decreases towards the neck to 1–3 layers. Its cells, regardless of their location in the layer, have a flattened shape and are oriented parallel to the surface of the tooth.
The most interesting morphological feature of the structure of the attachment epithelium is the arrangement of epithelial cells between two basement membranes. Epithelial cells are located on the basement membrane, connecting it with the lamina propria of the gingival mucosa. The surface cells of this epithelium provide attachment of the gum to the tooth surface using hemidesmosomes associated with a second (internal) basement membrane located between the tooth and the attachment epithelium.
Both basement membranes have a similar structure and consist of two zones:
– electronically transparent zone,
located at the base of the epithelial cells of the basal layer and called the transparent plate;
– electron-dense zone,
underlying transparent plate.
The plates contain type IV collagen, laminin, anchorin, and glycoproteins.
Epithelial cells connected to the inner basement membrane do not undergo desquamation, which is not typical for stratified squamous epithelial cells.
Desquamation is experienced by cells lying under the surface layer of the attachment epithelium, which are displaced towards the gingival sulcus and then desquamated into its lumen. The intensity of this process in the attachment epithelium is 50-100 times greater than desquamation in the gingival epithelium.
The loss of cells is compensated by their intensive new formation in the basal layer of the epithelium, the cells of which are characterized by very high mitotic activity. From the basal layer, cells move simultaneously towards the enamel and gingival sulcus.
Typically, the rate of renewal of the attachment epithelium in humans is 5–8 days, and if damaged, its complete recovery occurs within 5–6 days.
In terms of their ultrastructure, the cells of the basal layer of the attachment epithelium are somewhat different from the epithelial cells of the rest of the gum.
The cytoplasm of cells contains a well-developed granular endoplasmic reticulum and a pronounced Golgi complex, while tonofilaments occupy a significantly smaller volume in it.
The composition of cytokeratin intermediate filaments of the cytoplasm, as well as surface membrane carbohydrates, characteristic of poorly differentiated cells, indicates the presence of attachment of this class of cells in the epithelium. In this regard, a number of researchers suggest that maintaining attachment epithelial cells in a relatively undifferentiated state is important to preserve their ability to form hemidesmosomes, which ensure the connection of the epithelium with the tooth surface [66, 85].
The number of desmosomes connecting cells of the attachment epithelium is 3–4 times less than in the furrow epithelium. In this regard, the intercellular spaces are usually expanded, they contain cells such as granular leukocytes, monocytes and lymphocytes migrating to the surface from the lamina propria. At the same time, many substances are transferred through wide intercellular spaces in the opposite direction from saliva and the oral cavity (bacteria, bacterial toxins, other antigens), which may be necessary for adequate stimulation of the immune system.
Own record
The gum consists of papillary and reticular layers.
The papillary layer is formed by loose, unformed connective tissue containing a large number of blood vessels and nerve fibers with numerous nerve endings. The high papillae of this layer are smoothed in the area of the gingival sulcus.
The reticular layer is represented by dense connective tissue with a high content of collagen fibers, bundles of which firmly attach the gum over its greater extent to the periosteum of the alveolar process (attached gum). On the other hand [21], the supra-alveolar zone of the lamina propria of the gum contains functionally oriented bundles of collagen fibers that form fibrous ligaments in the gum (Fig. 119):
– vestibular-oral fibers (fibrae gingivales vestibulo-orales) are located along the midline, moving in the interdental spaces from the vestibular surface of the gum to the oral one;
– dentogingival fibers (fibrae dentogingivales) start from the cementum of the root at the bottom of the gingival sulcus and spread fan-shaped into the connective tissue of the gums. The bundles are well expressed on the vestibular and oral surfaces, weaker on the contact surfaces;
– spiral interdental fibers (fibrae interdentales spirales) begin in the gum at the bottom of the gingival groove on the medial surface of the tooth, surround it in the form of a spiral and are woven partly into the cement of the same tooth on the distal surface, partly on the medial surface of the adjacent tooth;
– interdental fibers (fibrae interdentales) form bundles 1.0–1.5 mm thick, running from the cement of the contact surface of one tooth through the interdental septum to the cement of the adjacent tooth. They continue to the roots (interroot fibers). this group of fascicles plays a special role in maintaining the continuity of the dentition. They are involved in the distribution of chewing pressure within the dental arch;
– dentoperiosteal fibers (fibrae dentoperiostales) pass from the neck of the tooth to the periosteum of the jaws. In the area of incisors and canines, these fibers are better expressed on the contact surfaces, and in premolars and molars they are well expressed on all sides.
Some of these ligaments are part of the periodontal membrane.
The lamina propria of the mucous membrane in the area of the dental-gingival junction is characterized by the following:
– relative paucity of collagen fibers and fibroblasts;
– an extensive network of blood vessels;
– high content of leukocyte cells.
Rice. 119. Gingival ligaments (scheme according to S.S. Mikhailov).
I – medial root of the second molar: II – distal root of the second molar; III – root of the third molar
1 – dentogingival fibers; 2 – spiral interdental fibers; 3 – interdental fibers; 4 – vestibular-oral fibers; 5 – circular fibers; 6 – interroot fibers.
Granulocytes (mainly neutrophils), lymphocytes and monocytes are continuously evicted from the lumen of numerous vessels, which move through the intercellular substance of the connective tissue towards the epithelium and ultimately enter the gingival sulcus and then into saliva.
Thus, the gums are one of the main sources of leukocytes found in saliva and transformed into salivary corpuscles. The number of leukocytes migrating through this route into the oral cavity is normally about 3000–5000 per minute. Most of them (70–90%) have high functional activity in the initial period after migration.
With pathology, the number of migrating leukocytes increases significantly. It is believed that the rate of movement of leukocytes is influenced by chemotactic factors secreted by bacteria that are located in or near the gingival sulcus.
Thus, such a high content of leukocytes is necessary to protect the relatively thin and non-keratinizing epithelium of the gingival sulcus and attachment epithelium, as well as the underlying tissues, from the penetration of microorganisms from the oral cavity.
All problems can be solved
An even dentition, white teeth of regular shape adorn any person and serve as an integral part of an ideal smile. Thanks to this, everyone can feel attractive, because in the modern world almost any dental defect can be successfully corrected. Thanks to this, many patients are able to return to normal life. Therefore, if you are concerned about the presence of a diastema, this imperfection can be corrected quite quickly and painlessly in dentistry near the Krasnye Vorota, Baumanskaya, Novokuznetskaya and Tretyakovskaya metro stations. Do not be indifferent to your health and psychological state, and confidently contact dental specialists to solve your problems.
Diastema in celebrities
Teeth are the calling card of any famous person, and, according to many, they must be perfect. But there are many stars who have turned the gap between their teeth into their highlight. According to physiognomy, gaps between teeth are a sign of talent and creative potential.
Famous women with diastema
To the list of stars with diastema who became famous in the last century, in addition to Brigitte Bardot and Ornella Muti, you can add Lauren Hutton, who conquered the fashion industry back in the 60s of the 20th century. Among modern models is Georgia May Jagger, who became the face of the Chanel advertising company.
Diastema makes French celebrities even more attractive and is an integral part of their image. In addition to Vanessa Paradis with her pronounced diastema, one can remember the actress Jane Birkin, who considered the gap to be a “funny little thing.” Léa Seydoux, the performer of the role of Belle from Beauty and the Beast, is in no hurry to get rid of this defect.
American women are more conservative in this regard and strive for a Hollywood smile. Fifty Shades of Gray star Dakota Johnson once had a great sense of humor about her diastema. To be convinced of this, just watch a video of a famous American television show with her participation. But over time, the actress got rid of her diastema.
Famous men with diastema
Diastemas and trema in famous men are quite common. Among Hollywood veterans who got rid of the gap between their teeth, we note Arnold Schwarzenegger, Tom Cruise, Nicolas Cage. But the famous director Oliver Stone did not treat the diastema. The gap does not prevent Woody Harrelson, Eddie Murphy, and Laurence Fishburne from smiling widely.
Among the representatives of the younger generation who corrected diastema in their youth, we highlight Zac Efron and Matthew Lewis.
Johnny Depp and the cult director Tim Burton uniquely expressed their “love” for gap teeth by creating the image of the Mad Hatter in the film “Alice in Wonderland.”
You can have different attitudes towards diastema and trema, but you shouldn’t deny that they really suit some of the stars. Diastema can highlight a bright appearance and make it memorable.