From this article you will learn:
- what are gum diseases,
- how do they differ from each other,
- treatment and symptoms of gum disease in adults.
The article was written by a dentist with more than 19 years of experience.
Gum disease is a whole group of diseases, among which the most common are “gingivitis” and “periodontitis”, and much less frequently are diseases such as periodontal disease. The latter term is known to everyone, but in most cases patients use it incorrectly, using it to refer to inflammation of the gums. Although real “periodontal disease” occurs without inflammation at all and is only a degenerative gum disease.
In professional language, gum disease is usually called “periodontal disease,” and dentists who specialize in the treatment of this pathology are proudly called periodontists. Therefore, if you have one of the gum diseases, we recommend that you contact periodontists for advice and treatment, and not regular dental therapists. The same applies to regular removal of dental plaque.
What is periodontium (periodontal disease) –
This is a complex of tissues surrounding the tooth, which includes - 1) the gums around the tooth, which is part of the mucous membrane of the oral cavity, 2) periodontium - the ligamentous apparatus due to which the tooth is attached to the bone, 3) the bone tissue around the tooth. In accordance with the fact that various gum diseases are accompanied by inflammation and/or destruction of the constituent parts of the periodontium, these diseases are called the specific term “periodontal diseases”.
In addition to gingivitis, periodontitis and periodontal disease, periodontal diseases include 2 more groups of diseases. Firstly, quite rare “idiopathic periodontal diseases” (these include desmontosis, histocytosis-X and Papillon-Lefevre syndrome). Secondly, these are benign tumor-like formations, called “periodontomas”. These include, for example, diseases such as gingival fibromatosis, epulis and periodontal cysts.
Gum disease: symptoms and treatment
Gum diseases in adults and children occur in the same way. Below we will analyze each disease - with a description of its characteristic symptoms and photographs of the patients’ teeth and gums. The information will allow you to easily distinguish one disease from another, and understand how much professional treatment you will need in different situations.
The author of the article has more than 10 years of experience as a periodontist, and therefore our recommendations really work (state-issued documents on advanced training in the Periodontology program can be viewed in the editorial section).
Content:
- The most common gum diseases
- Why gum disease occurs
- How diseases manifest themselves
- Treatment
- Preventive measures
4.1. Oral hygiene 4.2. Physiotherapy 4.3. Anti-inflammatory drugs 4.4. Curettage 4.5. Surgery
Worried about the whiteness of their teeth and the aesthetics of their smile, people often forget about the health of their gums. Meanwhile, among other dental diseases, their pathologies provide significant competition to caries. Moreover, premature loosening and loss of incisors and molars is very often associated with infection of the apparatus that holds them.
Gingivitis –
Gingivitis is an inflammation of the gingival margin, including the interdental gingival papillae (i.e., that part of the gum that is directly adjacent to the necks of the teeth). The main symptoms of this disease are periodic bleeding and soreness of the gums when brushing teeth, redness or cyanosis of the gingival margin, swelling of the gingival papillae, and often there is bad breath. Gingivitis with a predominance of such symptoms is called “catarrhal” by dentists.
Gum disease: photo of teeth with gingivitis
The cause of the development of catarrhal gingivitis is exclusively insufficient oral hygiene. As a result, soft microbial plaque accumulates at the necks of teeth, and hard dental deposits can also form (we are talking about tartar). In this case, the development of inflammation is due to the fact that pathogenic bacteria that are part of microbial plaque and tartar secrete various toxins and inflammatory mediators, which trigger a chain of inflammatory reactions in the gums.
Therefore, the main treatment for inflammatory gum diseases is always aimed at eliminating the causative factor, i.e. for the removal of dental plaque (+ normalization of oral hygiene). It should be noted that gingivitis is the simplest and most quickly curable form of gum inflammation, if, of course, the treatment is carried out correctly - with regular removal of dental plaque by ultrasound (the frequency of this procedure will depend on the quality of the patient’s oral hygiene).
Important: inflammation in gingivitis affects only the mucous membrane of the gums - without destroying the dentogingival attachment or bone tissue around the teeth (which is typical for a more severe form of gum inflammation - periodontitis). But the transformation of gingivitis into periodontitis is only a matter of time if the patient focuses his treatment on antiseptic mouth rinses and gel applications on the gums, rather than on the removal of dental plaque and high-quality hygiene.
Hypertrophic form of gingivitis –
Catarrhal gingivitis is the most common form of gingivitis, but not the only form. Sometimes patients can experience a hypertrophic form of gingivitis, which is manifested by an increase in the volume of the gingival papillae or the gingival margin as a whole (usually only in the area of the front teeth). Most often, this form occurs in pregnant women and adolescents, and is associated with hormonal changes in the body. There are edematous and fibrous forms of hypertrophic gingivitis.
In the edematous form, the enlargement of the gingival papillae occurs due to their chronic persistent swelling, which is practically untreatable. This form can occur not only in pregnant women, but also in patients with long-term catarrhal gingivitis (in the absence of adequate treatment). In the fibrous form, gum enlargement occurs due to the proliferation of fibrous tissue (Fig. 4). You can read more about the forms of catarrhal and hypertrophic gingivitis and their treatment regimens at the link below.
→ Treatment of gingivitis in adults
Healthy gums contain a healthy tooth
Each tooth is surrounded by soft tissue. They carefully protect its vulnerable spots from bacteria, the mechanical effects of food and acidity surges. The collection of these tissues around each tooth is called the gum.
Let's imagine that:
- The oral cavity is a huge house in which teeth “live”.
- Each tooth has its own “apartment” - the gums.
A person feels better in a well-kept and renovated apartment. Let's make an analogy: teeth need healthy gums.
Let’s figure out what you need to be wary of and what to do if your fears become reality. Let's talk about the health of our gums.
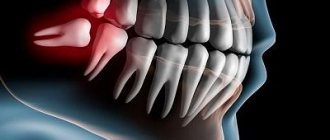
Periodontitis –
In the absence of treatment or improper treatment of catarrhal gingivitis, the latter inevitably turns into chronic generalized periodontitis. And if with gingivitis the inflammation covers only the mucous membrane of the gums, then with periodontitis there is a gradual destruction of the periodontal attachment, as well as the bone tissue around the teeth. As a result, over time this leads to tooth mobility and the need for their removal.
Gum diseases: photos of teeth with periodontitis
Periodontitis can be mild, moderate or severe. The symptoms of a mild form of periodontitis differ little from the symptoms of catarrhal gingivitis, and the patient in most cases will not notice that the condition of the gums has immediately “significantly worsened.” Vivid symptoms of periodontitis (mobility of teeth, their displacement, exposure of roots) become noticeable only in moderate and severe forms.
Differences between periodontitis and catarrhal gingivitis –
In addition to bleeding and sore gums, as well as swelling, redness or bluishness of the gums with catarrhal gingivitis, periodontitis occurs:
- destruction of the periodontal attachment,
- destruction of bone tissue and periodontal fibers, due to which the tooth is attached to the bone,
- formation of periodontal pockets (Fig. 6),
- presence of subgingival tartar,
- suppuration from periodontal pockets (during periods of decreased immunity),
- Over time, mobility and displacement of teeth appear.
Differences between periodontitis and gingivitis: diagram
With mild periodontitis, the depth of periodontal pockets is no more than 3.5 mm (and this still allows for very effective treatment and stabilization of the process). With moderate/severe periodontitis, the depth of periodontal pockets reaches 5-6 mm or more, and the amount of bone destruction around the tooth is such that mobility of first individual, and then most teeth appears. Further, under the influence of mechanical loads, the teeth begin to shift in different directions or fan out (Fig. 6-7). You can find out more about the symptoms of periodontitis and what it looks like on x-rays in the article at the link below.
→ Signs of periodontitis in adults
Important: over many years of working as a periodontist, I have seen thousands of patients with periodontitis, which always occurs for the same reason. The basis is always irregular and/or poor-quality oral hygiene, against which the patient has been using antiseptic rinses, gels and toothpaste for bleeding for many years (believing that this is the best and only protection against gum inflammation). Such patients spend a huge amount of time on various procedures, but cannot bring themselves to spend 3-4 minutes 3 times a day brushing their teeth after each meal (including the mandatory use of dental floss).
As a result, patients regularly “suppress” the symptoms of inflammation with the help of anti-inflammatory drugs, while toxins from microbial plaque and hard tartar continue to destroy the gums and their attachment to the teeth (this process is simply less noticeable). This is because most patients with periodontitis struggle exclusively with the symptoms of the disease (bleeding, swelling of the gums), and not with the cause of their inflammation - soft microbial plaque and tartar.
Local form of periodontitis –
In addition to chronic generalized periodontitis, with which most patients seek treatment for gum inflammation, there is also so-called localized periodontitis. The latter is characterized by the development of not all, but only 1-2 teeth in the area. It is caused by local reasons. This may be an overhanging edge of the filling in the interdental space, or a poorly placed filling on the side surface of the tooth (as a result of which there is no tight contact between the teeth in the interdental space).
This could be a traumatic bite, i.e. in the presence of so-called “super contacts” (when the teeth do not close at the same time, but there is premature biting on some teeth, which over time will lead to their mechanical overload). These can be poorly made removable dentures, as well as low-quality artificial crowns (24stoma.ru). The latter, like fillings, can either injure the gingival margin, or have supercontacts, or have poor contacts with neighboring teeth in the interdental spaces.
Treatment of localized periodontitis involves eliminating the traumatic factor. This may be expressed in the need to replace a filling, crown, prosthesis, or in the presence of supercontacts - in the need for “selective grinding of teeth.” The rest of the treatment is carried out only after the traumatic factor has been eliminated. It may include anti-inflammatory therapy, as well as curettage of the periodontal pocket.
Is gum grafting painful?
No . Operations to eliminate gum recession are performed under local anesthesia; the surgical intervention is 100% painless. In the postoperative period, especially with gum plastic surgery using local tissues, patients often do not experience pain at all. If pain occurs, it is usually only on the day of surgery, a couple of hours after the intervention, when the effect of the local anesthetic wears off. During this period, the pain is perfectly eliminated with painkillers prescribed by the doctor. During the entire rehabilitation period, on average, 1-2 painkiller tablets are required.
In cases of gum plastic surgery using a “patch,” unpleasant sensations may be added due to the presence of a donor zone, which, according to patients, resembles the feeling “as if you grabbed hot tea,” but this does not always occur. The presence/absence of pain is determined by the area from which the “patch” is taken. If anatomical conditions allow, doctors can remove the graft from the donor area absolutely painlessly.
Periodontal disease –
If gingivitis and periodontitis are interrelated and, in fact, are successive stages of the inflammatory process, then periodontal disease is a completely special disease. It is not based on an inflammatory process, but on neurotissue degeneration of all periodontal tissues (i.e. gums, periodontal tissue and bone tissue around the teeth). The mucous membrane of the gums with periodontal disease has no signs of inflammation - it is pale pink, dense, and there is no bleeding of the gums when brushing.
Photos of teeth and gums with periodontal disease –
The main reason for the development of tissue dystrophy (periodontal disease) is age-related changes in blood vessels, and that is why this disease can most often be found in pensioners. It should be noted that with age, the vessels become sclerotic (their lumen decreases), and as a result, the blood supply to the bone and soft tissues of the gums, their saturation with nutrients and oxygen, deteriorates. This causes the development of sclerosis and bone tissue atrophy, which is visually manifested by a decrease in the height of the gums and exposure of the roots of the teeth.
An interesting point in the development of periodontal disease is the lack of mobility of the teeth, even with a significant loss of bone tissue around them. Studies have shown that this is due to a significant decrease in the thickness of the periodontium (due to which the tooth is attached to the bone tissue), as well as due to a qualitative change in the connective tissue, which is gradually replaced by simple fibrous tissue. As a result, the tooth becomes tightly fused with the bone.
Important: as you already understand, most patients incorrectly call any gum disease “periodontal disease.” And in 99% of cases, these patients have periodontitis, which occurs with periodic exacerbations of the inflammatory process, the gums are loose, often bleed when brushing, there is always swelling and cyanosis of the gingival margin (not to mention periodontal pockets with purulent discharge and tooth mobility).
With periodontal disease, the gums are always pale pink, dense, and tooth mobility (unlike periodontitis) develops only when the level of bone destruction reaches more than 1/2 the length of the tooth roots. The diagnosis can be confirmed by x-ray - with periodontal disease, the image will clearly show areas of bone tissue sclerosis (its compaction), and not areas of inflammatory resorption, which are observed with periodontitis.
Other signs that distinguish periodontal disease from periodontitis –
In doubtful situations, the following 2 signs can help to diagnose periodontal disease. Firstly, with periodontal disease there is always a delay in the abrasion of the cusps (on the chewing surfaces of the teeth). The second point is the presence of a large number of wedge-shaped defects in the neck area of the teeth.
Difficulties in diagnosis can occur when poor hygiene is combined with periodontal disease, and then the patient experiences symptoms of catarrhal gingivitis (swelling of the gums, bleeding when brushing) on top of the symptoms of periodontal disease. But removing dental plaque and teaching oral hygiene quickly returns clinical symptoms to the original basic disease.
What are the recommendations and restrictions after gum recession surgery?
- Do not disturb the wound surface (with tongue, food, foreign objects, etc.) this is the main condition for good healing.
- Do not bite (food eaten should be soft or finely chopped).
- Do not brush your teeth in the surgical area with a toothbrush (hygiene in this area should be maintained only as permitted by the attending physician).
- Do not eat or drink hot foods.
- Avoid physical activity.
- Follow the recommendations of your doctor and take prescribed medications.
Gum disease: treatment
It is unfortunate, but the most adequate patients who follow absolutely all the recommendations of a periodontist are those who have self-medicated for a long time with various rinses, ointments, and also used different toothpastes “for the gums.” When such patients come with loose teeth and suppuration from periodontal pockets, they no longer need to be convinced: 1) of the ineffectiveness of such self-medication, 2) of the need to regularly spend money on removing dental plaque, 3) of the need to brush their teeth after every meal, including flossing rather than twice a day.
Yes, such patients have a difficult situation in the oral cavity, but they are easy to work with. And when, after just a few days of adequate therapy, they see the first positive results, and you further recommend splinting their mobile teeth with fiberglass or curettage of periodontal pockets - they sign up without any questions and do it. But there are other patients for whom “not everything is so bad,” and who almost always listen with distrust to your recommendations - remove dental plaque, do curettage, splinting, prosthetics. They always think that they are being deceived and cheated out of money, and finally they always ask “how much does it cost” and then disappear for 1-2-3 years.
When they come again, they are also ready to do anything to avoid having their teeth removed and wearing removable dentures, but in many cases this is all that remains to be done. Therefore, when reading this article, you have 2 choices. The first option is that you can take only the anti-inflammatory therapy regimen for yourself, and then treat yourself at home. The second option is to also undergo a course of home anti-inflammatory therapy, but before that, visit a periodontist at least to remove the causative factor of gum inflammation, i.e. supra- and subgingival dental plaque.
Important: remember that gingivitis is reversible, and its proper treatment leads to a complete cessation of inflammation in the gums, and if after treatment, oral hygiene is good and regular, then you will never have gingivitis again. The development of periodontitis begins with the destruction of the dentogingival attachment (i.e., the attachment of the gingival margin to the necks of the teeth). As soon as the fibers of this attachment are destroyed, a path is opened for pathogenic bacteria under the gum, and there they do what they do best - they begin to destroy bone tissue, as well as the periodontal attachment (due to which the roots of the teeth are attached to the bone).
It is no longer possible to restore the destroyed dentogingival attachment and periodontal attachment. The resulting periodontitis can only be stabilized at the stage at which you consulted a doctor. Below we will talk about the general principles of treating gum disease, and you will also find useful links where some treatment issues are discussed in much more detail (than in this review article).
How to treat gums with gingivitis -
In general, you need to start with a consultation with a periodontist, and if periodontal pockets are found during the examination, the doctor will refer the patient to a panoramic photograph of the teeth - with a preliminary diagnosis of “chronic generalized periodontitis.”
If a diagnosis of “catarrhal gingivitis” is made, then this is a reason for joy, because in this case, treatment will consist only of removing dental plaque, a short course of anti-inflammatory therapy, as well as training in oral hygiene. Removal of microbial plaque and tartar is most often carried out using ultrasonic cleaning. This is a completely painless procedure, provided there is no increased sensitivity of the necks of the teeth (otherwise, anesthesia may be required). Usually, with gingivitis, only 1-2 visits to the periodontist are enough, who will remove dental plaque, polish your teeth, and also prescribe antiseptic rinses and gel applications to the gums. Well, he will definitely teach you how to use dental floss and brush your teeth correctly.
Video of dental plaque removal with ultrasound –
Anti-inflammatory therapy –
Anti-inflammatory therapy is prescribed by the dentist immediately after ultrasonic teeth cleaning, and its duration will be 7-8 days for the treatment of catarrhal gingivitis, and 10 days for periodontitis. In most cases (with the exception of patients with purulent discharge from periodontal pockets), there is no need to carry out antiseptic rinses and treat the gums with gel at a dentist’s appointment; you can do this just fine at home.
The procedures are carried out 2 times a day - in the morning and in the evening (after breakfast/dinner and subsequent oral hygiene). Please note that the sequence should be “breakfast → brushing teeth”, and not vice versa. First, you should perform an antiseptic mouth rinse with chlorhexidine solution. Depending on the severity of gingivitis, the effective concentration of chlorhexidine should be from 0.12 to 0.25%, but if we are talking about periodontitis, then rinsing your mouth with only 0.2-0.25% chlorhexidine.
Why exactly these concentrations - you can read at the link above, and in the same article you will find information on specific mouthwashes that contain chlorhexidine in this concentration. To rinse, you need to put 10-12 ml of solution in your mouth (this is about 1 sip) and, without spitting, rinse your mouth for 1 minute. After spitting the solution, it is important not to rinse your mouth with water! And then you will need to apply an anti-inflammatory gel to the gums.
Gel application regimen - I have treated thousands of patients with gingivitis and periodontitis, and in my opinion, the most effective anti-inflammatory gel is the drug Cholisal. If its price is high for you, then an alternative may be Parodontocid gel (however, it will work effectively only if used with antiseptic rinses, where the concentration of chlorhexidine will be at least 0.2%).
Before applying this gel to the gums, it is advisable to dry the wet mucous membrane of the gums using a dry gauze pad, because in this case the gel will stick better. Apply the gel only in front of a mirror, with your teeth bared properly (so that you can clearly see the gingival margin around the necks of the teeth). The gel should be applied only to the marginal part of the gum around the teeth, i.e. on the gingival margin - using a clean finger. To do this, you will squeeze portions of the gel onto the tip of your index finger and transfer the gel from it to the gum.
It is optimal to first treat the gums around the lower teeth, and then around the upper ones. On the gingival margin from the front surface of the teeth, the gel is best applied in 2 stages. First, rub small portions of the gel with light massaging movements, after which the second stage is to apply the gel without massage and leave it on the gum. On the palate/tongue side, it is also advisable to apply the gel, but here it is enough to only rub in small portions of the gel.
Important: we draw your attention to the fact that saliva will always be released during the application of the gel, but it does not need to be accumulated in the mouth or specially spit (swallow it as usual). In addition, after treating the gums with gel, it is undesirable to drink for 30-40 minutes, and it is also undesirable to eat or not rinse your mouth for 2-3 hours. The second treatment should be carried out in the evening according to a similar scheme (dinner → oral hygiene → antiseptic rinse → application of gel to the gums). And so on for 7-8 or 10 days, depending on the type of gum inflammation.
Useful links -
→ The best mouthwashes, → Rating of the best gels for gums.
Oral hygiene training –
Remember that the effect of treatment will not last long if you continue to not floss and brush your teeth after every meal. You can see how to brush your teeth correctly in the following video, and you will find comprehensive recommendations on oral hygiene in the article, the link to which is under the video.
→ Detailed recommendations for oral hygiene
How to treat gums with periodontitis -
You need to start with a consultation with a periodontist and analysis of a panoramic X-ray. Basic therapy will continue to consist of removing dental plaque and anti-inflammatory therapy, which may additionally include systemic antibiotic therapy. Periodontitis differs from gingivitis by the presence of not only supragingival, but also subgingival dental deposits, which are localized in periodontal pockets.
The problem is that not only ordinary dentists, but even many periodontists remove subgingival deposits quite poorly. The fact is that searching for subgingival dental plaque and removing it requires a large amount of doctor’s time (much more than for removing supragingival dental plaque), and time in modern dentistry is money. Therefore, with moderate/severe periodontitis, even 3-4 visits to the dentist may be required for high-quality removal of deposits. Removal of plaque is usually carried out using ultrasound (ultrasonic scaler), but we do not recommend using the Vector system apparatus for primary removal of dental plaque.
Depending on the degree of destruction of bone tissue and the depth of periodontal pockets, splinting of mobile teeth, depulpation of teeth, removal of highly mobile teeth, curettage of gum pockets, prosthetics of missing teeth, etc. may be required. Thus, further treatment for each patient will be individual, depending on the specific situation in the oral cavity. Read more about special additional treatment methods in the article:
→ Treatment of moderate and severe forms of periodontitis
How to treat gums with periodontal disease -
Treatment of this form of the disease is fundamentally different from the treatment of gingivitis or periodontitis. because The cause of periodontal disease is tissue degeneration and sclerosis, and not microbial factors and inflammation. The main treatment will be aimed at stimulating blood circulation in the gums (primarily physiotherapeutic methods are used for this), as well as at normalizing occlusal contacts between the upper and lower teeth.
Effective methods of physiotherapy for periodontal disease -
- vacuum massage of gums (including creation of vacuum hematomas),
- electrophoresis of drugs,
- the use of diadynamic currents,
- use of helium-neon laser.
All of the above methods are carried out only in a physiotherapy office; your dentist can give you a referral for the procedure. In addition to physiotherapeutic methods, regular massage of the gums, which can be done with a finger, can have an effect. An additional effect can be provided by regular courses of using Asepta gel containing beekeeping products, which will improve blood circulation in the gums.
How modern clinics save gums
The treatment is carried out by a periodontist. It can be found in any dental clinic. We recommend visiting the dentist once a year. Treatment consists of several stages:
- Elimination of the cause of the disease,
- Anti-inflammatory therapy,
- Dental fixation, removal,
- Further prevention.
The cause of inflammation is eliminated by cleaning the oral cavity using various methods.
Previously, doctors practiced the instrumental method of removing plaque. Now – sandblasting and ultrasonic cleaning. These 2 methods are used together. First, stronger ultrasonic cleaning occurs, then cleaning with compressed air moistened with solutions of special salts. In severe cases, it is recommended to carry out procedures once a quarter.
Air Flow Treatment
This is a modern version of sandblasting the oral cavity. Suitable for removing soft plaque. More durable deposits are resistant to this cleaning method. Sodium bicarbonate (baking soda) is used as salt in combination with other substances. The mixture is under enormous pressure, so the output is a powerful stream that dissolves and washes away plaque.
Ultrasonic cleaning of the oral cavity
This is the best method of all time. The principle of the method: dental stone and plaque are destroyed by ultrasound. The nozzle of the device is generously moistened with a stream of antiseptic solution or purified water to wash off the crushed plaque.
Then each tooth is ground with a special attachment.
As an example, let's talk about the drug Vector. This is a German technology for ultrasonic cleaning of plaque. A special feature of the device is the direction of the sound wave along the tooth. With the help of Vector, plaque is removed faster and more efficiently than using non-directional ultrasonic vibrations.
Anti-inflammatory therapy
It consists of using gels and special pastes. The most common method is the complex use of cholisal dental gel (pain relief), an antiseptic solution (chlorhexidine or chlorophyllite), and paste to maintain healthy gums (lacalut, paradontax). It is recommended to use this treatment tactic for 21 days after the procedure.
In the case of gingivitis, treatment ends at this stage.
Be sure to read our article about periodontal mouthguards “New in gum treatment”
Surgical intervention, splinting, prosthetics
In case of periodontitis, further therapeutic measures are required: the patient is prepared for prosthetics or splinting (loose teeth are attached to a healthy dental mass using a splint).
Treatment should be accompanied by taking antibacterial drugs!
Surgical cleaning of periodontal pockets is the main method of treating periodontitis.
The operation is performed under local anesthesia and lasts less than an hour. The most common method of cleaning pockets is the “flap operation.” The gum is cut into flaps, which are sewn back after cleaning. Hence the name of the manipulation.
Modern anesthesia allows invasive interventions to be performed absolutely without pain.
Why you can’t self-medicate
Home treatment – eliminating symptoms! The cause of the disease remains, but the pathological process will remind itself again and again and develop further. It is necessary to eliminate the cause, which cannot be done at home.
Important for patients with cardiovascular pathology -
Many patients with gum inflammation try to self-treat, which involves regular use of antiseptics. Antiseptic solutions are not able to completely “disinfect” dental deposits (consisting of pathogenic bacteria) - to their entire depth, because antiseptics affect only the most superficial layer of microbial plaque or tartar. Therefore, firstly, the pathogenic effect of bacteria will continue even against the background of antiseptic rinses. But this is not the most dangerous thing.
Scientific research has shown that antiseptics interfere with the ability of oral bacteria to convert nitrates (found in foods) into nitrites. This bacterial activity is called “nitrate-reducing” and is one of the mechanisms that regulates our blood pressure. The fact is that nitrites formed by bacteria are then absorbed into the blood, and they help lower blood pressure. Therefore, if you regularly use antiseptic products (even toothpastes), this will reduce the production of nitrites by oral bacteria and may cause an increase in blood pressure.
This may not be noticeable in young healthy people, but will be significant in patients with chronic cardiovascular pathology. All these data are confirmed by scientific research - “The increase in plasma nitrite after a dietary nitrate load is markedly attenuated by an antibacterial mouthwash. Nitric Oxide" (2008), authors – Mirco Govoni, Emmelie Å. Jansson, Eddie Weitzberg, Jon O. Lundberg. If you wish, you can read this study using the link above using a browser translator. We hope that our article was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a periodontist, 3. American Academy of Periodontology (USA), 4. “Therapeutic dentistry. Textbook" (Borovsky E.V.). 5. “Non-surgical periodontal treatment” (Roncati M.).
What are the features and complications after gum recession surgery?
With a mild course of the rehabilitation period, patients do not note any peculiarities . But sometimes it is possible:
- the appearance of white plaque on the gums (this is normal, one of the healing options after gum surgery).
- swelling of the soft tissues of the face (from minor swelling to significant) depending on the extent of the surgical intervention (number of teeth involved), the size of the recession, the method of its closure, anatomical features and the patient’s body.
- hematomas on the facial skin (rarely encountered with gum surgery).
- increase in body temperature.
- pain (relieved by painkillers).