Tooth dislocation is a displacement of the tooth position in one direction or another, the direction of which depends on the direction of the impact force (impact). Dislocations of primary teeth are approximately three times more common than similar injuries to permanent teeth; this is due to the lower stability of primary teeth in the jaw bone.
Not all situations can be foreseen; if an injury occurs, you need to remember that the treatment of each type of dislocation has its own characteristics, and seeking dental care as soon as possible increases the percentage of favorable outcomes.
Causes of dislocations
Dislocation always occurs under the influence of a directed force, the source of which is:
- a blow to the tooth during a game, a fall, a fight, an accident, an industrial accident;
- the load acting on the tooth when chewing bones, unshelled nuts, or opening beer bottles with the teeth;
- incorrect tooth extraction technique;
- pressure on a moving tooth when biting hard food.
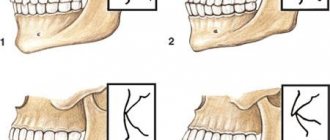
When dislocation occurs, the position of the tooth root in relation to the walls of the socket changes, periodontal fibers are completely or partially torn, and the neurovascular bundle is damaged; often a dislocation is combined with a fracture of the tooth crown or maxillofacial injuries. Based on the nature of tooth displacement, incomplete, complete and impacted dislocations are distinguished.
What causes malocclusion to form?
Defects appear for various reasons:
- Genetic predisposition. In most cases, mesial and distal bites are inherited. Therefore, parents who have this problem should take their child to an orthodontist in early childhood.
- Anomalies of fetal development. A child’s teeth are formed while still in the womb. During a complicated pregnancy or the influence of negative factors on its course, anomalies of the dental system can form.
- Birth injury. Mesial bite in some cases is a consequence of dislocation of the baby’s lower jaw during childbirth.
- Bad habits. Constant thumb or pacifier sucking, improper latching of the nipple, incorrect sucking during artificial feeding - all this provokes the development of malocclusion pathologies.
- Inferiority of the dentition. You can resort to removing baby teeth if there is less than a year left before the change. Otherwise, the dentition becomes asymmetrical, the midline shifts, and the chewing movements of the jaw are blocked. The formation of a permanent bite ends at approximately 15 years of age. For adults, after tooth loss, it is important to undergo prosthetics in a timely manner.
- Displacement of the jaws as a result of hypertonicity of the masticatory muscles, which can be observed due to stress.
Jaw injuries, as well as improper prosthetics, can provoke the development of malocclusions.
Symptoms and treatment of dislocations
Incomplete dislocation
With incomplete luxation, the tooth changes its position in the dentition in some direction, and its root moves. The tooth becomes mobile, patients experience pain that intensifies when eating. The gums around the dislocated tooth swell and bleed slightly. Due to the incorrect position of the tooth, the patient cannot close his jaw and keeps his mouth slightly open.
Treatment for incomplete dislocation of a permanent tooth consists of repositioning, that is, installing the tooth in its normal position. The manipulation is performed after applying local anesthesia: the dentist wraps his fingers around the dislocated tooth and carefully returns it to its place. After this, splinting is performed - a splint is installed on the injured and adjacent teeth, which fixes the tooth in the correct position and protects it from stress.
After installing the splint, the viability of the pulp is determined; if it dies as a result of a strong blow, depulpation is carried out.
Treatment for an incompletely luxated primary tooth with minor displacement involves returning the tooth to its correct position and monitoring the patient. If the tooth is severely displaced, it must be removed.
Complete dislocation
Complete luxation – loss of a tooth from its socket; patients experience severe pain, the socket bleeds, there are often wounds or bruises on the face, or traumatic brain injury.
Patients often believe that if a traumatic tooth loss occurs, nothing can be done. But there is a chance of restoring a lost tooth using the replantation method - with prompt action by the patient and the doctor, the tooth returns to the socket. This applies only to permanent teeth; replantation of milk teeth is not carried out.
The success of the operation depends on the correct behavior of the patient:
- the knocked out tooth needs to be found;
- place in a medium close to physiological (sodium chloride solution 0.9%, milk); In this case, the tooth cannot be wiped or touched by the root;
- come to the dentist immediately.
Reducing the time period from the moment of injury to replantation increases the chances of tooth engraftment. When a permanent tooth with formed roots is completely dislocated, the pulp dies, so it is removed some time after replantation. Sometimes the pulp is removed before the tooth is returned to its socket.
The pulp of teeth with an unformed root has the property of revascularization - restoration of blood vessels in it, therefore, when replantation is carried out as soon as possible after injury, it is possible to preserve the viability of the pulp. If this does not happen, depulpation is performed.
If replantation is not possible, after the hole has healed, prosthetics are performed to restore the integrity of the dentition. Prosthetics in childhood are performed if there is a recommendation from an orthodontist, under whose supervision the child must be kept after tooth loss.
Impacted dislocation
This type of dislocation is characterized by the immersion of the tooth into the socket, while the root penetrates into the bone tissue of the jaw, destroying the bottom of the alveolus. The tooth may be displaced away from its axis; traumatic injuries to adjacent teeth and oral mucosa are often detected; Traumatic brain injury may be present. Severe pain, swelling of the gums, and bleeding appear. Sometimes the tooth is driven in so deeply that it is not visually identified in the socket.
Treatment of impacted dislocations depends on whether the temporary or permanent tooth was injured. Temporary teeth with unformed roots with a small degree of intrusion can independently fall into place. If the teeth do not move forward within six weeks, they are removed. Injured baby teeth with formed roots are also removed.
If a permanent tooth with an unformed root is injured, it can also move into place on its own. If this does not happen, the tooth is placed in the correct position using orthodontic appliances. Reposition of teeth with a formed root is carried out immediately after injury or within 3 days, followed by splinting; It is possible to stretch the tooth using orthodontic appliances.
Correct bite: what is it like?
Bite is the way the teeth of both jaws interact when they are completely closed. If it is correct, there are no difficulties when chewing and pronouncing sounds, the aesthetics of the smile is not impaired, but minor defects are still possible. What does a bite that does not require orthodontic treatment look like? Its main characteristics:
- Presence of 28–32 teeth. Not all people develop “eights”, which is determined by genetic factors. Their presence (if they have grown correctly) or absence does not affect the closure of the jaws. Moreover, in some cases, wisdom teeth removal is indicated during orthodontic treatment. Then there is more free space in the mouth.
- Symmetry in the closure of the dentition.
- The incisors of the upper jaw overlap the lower ones by one third.
- No interdental gaps, cracks or chips.
- Correspondence of molars and premolars of both dentitions to each other. Their closure is tight.
- Ease of chewing food, even hard ones. Opening the mouth is easy and there is no pain.
Correct bite does not always look aesthetically ideal. But the face is harmonious.
Methods for diagnosing dislocations
When diagnosing dislocations, the following methods are used:
- Questioning the patient - the circumstances of the injury and the time when it occurred are clarified. The patient describes his feelings and complaints.
- External examination - the doctor assesses the general appearance of the patient, notes damage to the soft tissues of the face that occurred as a result of injury. The dentist may be the first to notice signs of a traumatic brain injury in a patient: pallor, sluggish reaction, weakness, respiratory rhythm disturbances.
- Examination of the oral cavity using a dental probe and a dental mirror. The mirror allows you to see areas that are not accessible to direct visual inspection. With the help of a probe, in case of incomplete dislocation, the depth of the periodontal gap is determined.
- Percussion - tapping on the tooth, helps determine the condition of the periodontium. In case of incomplete dislocation, percussion of the injured tooth causes acute pain; with impacted dislocation, percussion is painless or slightly painful.
- Palpation - feeling. Palpation of the gums with impacted dislocation is painful; Using this method, the dentist distinguishes incomplete dislocation from a root fracture.
- EDI – electroodontodiagnostics – determines the electrical excitability and conductivity of the pulp. A current of a certain strength is passed through the tooth using a special apparatus, and the patient is asked to report the tooth’s reaction to electrical impulses. If the pulp is viable, a slight feeling of pain appears in the tooth; When the pulp dies, there is no pain, the patient will feel a push in the tooth. During diagnosis, the threshold response of the tooth to current is recorded; in the normal state of the pulp, it is within the range of current readings from 2 to 6 μA.
Immediately after the injury, the pulp may not react to the action of the current, so tests are carried out 2-3 days after it, then every week for 4 weeks, sometimes longer. This is explained by the fact that while maintaining the viability of the pulp in case of dental trauma, its electrical sensitivity can be restored for a long time.
- X-ray examination - allows you to assess the condition of the roots of the tooth, periodontium, alveolar walls, jaw bone after injury; see the degree of tooth displacement after dislocation. It is preferable to carry out 3D computed tomography, since this method allows you to view the tooth and jaw bones in three projections, eliminating the effect of overlapping images.
- Transillumination diagnostics - transillumination of the tooth with a beam of cold light. Used to detect enamel cracks that cannot be detected with the naked eye. The method helps to maintain the health of teeth adjacent to the injured one, and at first glance not damaged during the injury.
Types of correct bite
The above describes the orthognathic bite, which is the reference. It occurs in only 5% of people. But there are other types of teeth closure in which violations are not detected. What does each one look like? Experts identify the following bites:
- Biprognathic. Both jaws are slightly pushed forward, and the teeth are slightly directed towards the lips.
- Opisthognathic. The opposite of the previous type. The teeth are directed inward. Opisthognathic occlusion is rare. Its features are noticeable when viewed in profile.
- Progenic. The lower jaw protrudes slightly, but this feature is not pathological. The functioning of the temporomandibular joint (TMJ) and the functionality of the teeth are not impaired.
- Straight. The upper row of teeth is parallel to the lower one. The incisors touch their cutting edges. This feature is not a deviation, but it threatens rapid wear of the teeth due to increased load.
Sometimes, if you have one of these malocclusions, minor adjustments may be needed. But the treatment in this case will be easy.
Additional treatments
Drug therapy
- When carrying out manipulations to reposition a tooth after dislocation, local anesthesia is used, for this purpose Ultracaine D-S, Ultracaine D-S Forte, Cytokartin, Septanest, Bupivacaine are used. But the effect of the anesthetic stops after some time, so painkillers from the NSAID group are prescribed: ibuprofen, nimesulide, ketorolac, dexketoprofen. Children are prescribed ibuprofen and paracetamol.
- To improve the condition of the gums after injury, use: Dentol Gel - has a local anesthetic effect.
- Gel Metrogyl Denta - contains two antibacterial components, eliminates inflammation.
- Kamistad gel is a combined drug: lidocaine has a local anesthetic effect, chamomile flower tincture produces antiseptic and anti-inflammatory effects, thymol has an antiseptic effect.
- Solcoseryl dental paste - stimulates regeneration processes in tissues, thereby shortening the healing period of wounds of the mucous membrane. The composition also includes polidocanol, a local anesthetic.
Physiotherapy
After acute phenomena have subsided, the following are used to stimulate healing processes and eliminate tissue swelling:
- UHF therapy is the effect on the body of an alternating electric field with ultra-high frequency.
- Microwave therapy – uses alternating electromagnetic oscillations of ultra-high frequencies of various ranges (centimeter, decimeter and millimeter).
- Magnetotherapy is the effect of a low-frequency magnetic field on the injured area.
- Magneto-laser therapy is a complex effect of magnetic and laser radiation.
Preventive actions
As you know, preventing the onset of a disease is always easier and cheaper than treatment. To prevent the appearance of gaps between teeth, you must follow basic rules:
- control the habit of chewing hard objects (for example, seeds, nuts, crackers, threads, wire, etc.);
- carry out proper hygienic care of the oral cavity (to maintain the health of the gums and prevent the spread of bacteria, it is very important to brush your teeth correctly, carefully brushing not only the chewing units, but also the canines and incisors);
- Conduct timely examinations with a dentist (this allows you to diagnose any deviation in time and begin treatment at an early stage).
If the cause of the appearance of interdental gaps is a genetic predisposition, it is very important to begin correction as early as possible. Maximum effectiveness is possible during the period when the teeth are still mobile in the gums and can be rebuilt.
Now you know exactly how to remove the gap between your front teeth, what methods are used for this and how long it takes to eliminate the defect. All that remains is to consult with an orthodontist and, after examination and research, choose a method for eliminating the diastema that is right for you.
Prevention
Prevention of tooth dislocation includes:
- Explanatory work with employees of industries associated with increased injuries. Each employee is required to comply with safety regulations, which provide for an algorithm for performing certain actions and the use of protective devices.
- Explaining to parents and children the rules for arranging playgrounds and behavior on them, familiarizing themselves with possible types of injuries and methods of providing first aid if they occur. Parents should supervise young children during play.
- Educational work among the population about the need to comply with traffic rules by drivers and pedestrians, as this is necessary not only to reduce the level of injuries, but also to save lives.
- Compliance by medical personnel with the rules for performing dental procedures.
- Avoiding bad habits: you need to use special tools to open bottles and crack nuts.
- Avoiding situations that could lead to a fight; if it does occur, during it you need to tense your masticatory muscles and keep your teeth closed: this will help avoid not only dislocation of teeth, but also a fracture of the jaw.
- Providing a high level of protection for athletes involved in traumatic sports (hockey, boxing). For this purpose, helmets with full face protection and mouth guards are used (molded, which have a ready-made shape, and molded - after heating in hot water, they take the individual shape of the teeth).
Anomalies in the closure of teeth
Dental rows are not always placed correctly. How do you know when treatment is required? Depending on the type of malocclusion, the following signs of violations are distinguished:
- Distal - the upper jaw is more developed when compared to the lower jaw. She comes forward significantly.
- Mesial. The situation is the opposite of the previous case - the lower jaw is more developed. It may bulge forward slightly or strongly.
- Cross. With this pathology, there are interdental gaps. Part of the upper front teeth is behind the lower ones, and the other part is in front of them. Such a smile looks unaesthetic. As a rule, teeth grow in different directions.
- Deep – the upper row of teeth almost completely overlaps the lower one. If even more than 30% of the teeth are blocked, this is considered a pathology. But visually such a violation may not be visible.
- Open. When the jaws close, only the chewing teeth come into contact; pronounced gaps are visible between the front teeth. In some cases, it looks like an open mouth.
Whatever the diagnosis, any pathology must be treated.
In our Center, we apply the principles of an integrated approach when planning treatment.
For the process to be successful, the patient receives consultation from several specialists. The process involves an orthodontist, an implantologist, and an orthopedist. They draw up a joint treatment plan, taking into account the volume of the bone, the distance between the teeth for the implant and the crown. If you do not take into account these nuances, you will have to re-install braces.
Levin Dmitry Valerievich
Chief physician, Ph.D.
It is important to consider how long ago the tooth was removed:
- If a tooth has been missing for a long time, and the neighboring ones have changed position and left no room for an implant, orthodontic treatment is aimed at freeing up space for an artificial root and crown.
- If implantation is planned after the braces are removed, a spring is placed on the adjacent teeth to prevent them from approaching each other and to leave space for the implant.
- If an implant is already in place and its position interferes with tooth movement, orthodontic treatment becomes more difficult. When trying to move an artificial root, there is a risk of its rejection, the development of inflammation, and tissue injury.
Content:
- Why is there a problem?
- Other reasons
- Is it necessary to remove a loose tooth?
- How to save a loose tooth
Only children with primary occlusion can react calmly to a loose tooth. For everyone else, this is a serious problem that requires immediate dental attention. If measures are not taken in time, you may encounter partial edentia - the movable unit will simply fall out at some point, which will negatively affect the functioning of the maxillofacial apparatus and, of course, the appearance of the smile. You should not decide on your own whether to remove a loose tooth. Only a qualified dentist, after an in-person examination, can tell you what to do correctly in a particular situation. Today, thanks to a large number of innovative treatment techniques, doctors most often manage to save even loose units.