Skin damage and wounds are always unpleasant. What can we say about trophic ulcers - companions of severe varicose veins, which are characterized by very sluggish and slow healing due to impaired tissue nutrition. Solcoseryl can help heal such difficult lesions, as well as burns, frostbite, and eye damage.
- Solcoseryl ointment as a face cream
- How to use Solcoseryl and Dimexide for wrinkles
In what forms is the drug available?
The manufacturer produces Solcoseryl in the form of ointment and gel for external use, as well as ophthalmic gel. In addition, this drug is available in injection form.
The active substance in all cases is calf blood extract - hemoderivat. Auxiliary components for each of the release forms are individual. Thus, in addition to the active substance, the solution contains only water for injection, and, for example, the manufacturer adds a number of ingredients to the ointment: white petrolatum, methyl parahydroxybenzoate, cetyl alcohol, etc.
The uniqueness of the composition of solcoseryl
The ointment has a uniform, greasy texture; the color can vary from deep white to yellow, with a characteristic odor of broth and petroleum jelly.
The active components of solcoseryl include deproteinized (removal of proteins) hemoderivat from the blood of 3-month-old calves at a concentration of 2.07 mg/g. Auxiliary components are represented by methyl parahydroxybenzoate and propyl parahydroxybenzoate (preservatives), palmitic alcohol (emulsifier), white petrolatum (ointment base), water for injection (dissolution of dry dialysate).
An analogue of the drug is Actovegin ointment. These drugs appeared on the pharmaceutical market almost simultaneously and differ only in the manufacturer and price.
The main active ingredient of solcoseryl is a deproteinized hemoderivat, which is obtained by dialysis and subsequent ultrafiltration. During the production process, high molecular weight proteins are removed (deproteinization). This is a complex compound that includes natural low-molecular substances with a molecular weight of up to 5000 Da.
Such a unique composition cannot be reproduced in laboratory conditions. Basically, these are electrolytes, amino acids, nucleotides, nucleosides. The effectiveness of only some of these substances has been described and proven from a pharmacological point of view. However, in vitro tests have proven the effectiveness of solcoseryl in the treatment of damaged tissues and wound surfaces.
What kind of medicine is Solcoseryl?
The drug has a beneficial effect on tissue metabolic processes. It improves tissue nutrition in case of damage, and also activates repair and regeneration processes.
Solcoseryl in injection form is used for extensive circulatory disorders (diseases of peripheral veins and arteries, strokes), ointment and jelly are used to treat ulcerative lesions and slow-healing wounds, and the gel is an ophthalmic agent. Thus, each of the release forms performs its own task of restoring damaged tissue.
The rate of absorption and distribution of the drug in the body, as well as the route of its elimination, cannot be determined by methods usual in pharmacology due to the characteristics of the active substance.
According to the results of a study of the drug on animals, the pharmacological effect develops within half an hour after the bolus injection. The therapeutic effect lasts for 3 hours.
Facial rashes: how to control them
If you have ever suffered from acne, you will no longer be careless in choosing cosmetics. One word “comedogenic” and the cream is forgotten forever. Regular struggle with blackheads - closed comedones, but before dates or important meetings, as luck would have it, an unpleasant surprise always pops up, and on critical days, pimples are generally a common thing.
There are a lot of remedies in your arsenal: pharmacy, cosmetic, folk remedies, but none of them eliminates the symptoms once and for all. Your friends advise you to take nutritional supplements and go to the solarium; you are frantically looking for a sane cosmetologist who can prolong the unstable remission. Is acne really never going to be cured?
This is wrong. Acne can be treated quite successfully. If you have a severe or moderate form of the disease (“moderate” acne), consult a cosmetologist, preferably a cosmetologist-dermatologist. Now there are many professional anti-acne lines. Be prepared for long-term treatment with uneven dynamics: after 2-3 sessions, temporary deterioration is possible, but this does not mean that the therapy was chosen incorrectly. You may be offered a combination of external therapy and tablets.
Dermatologists' methods will be stricter. There is a protocol (systematically developed recommendations) for treatment - this is a combination therapy: external agents and tetracycline antibiotics for several months. In my opinion, this option should be chosen only in severe cases, when there are multiple inflamed pustules, cystic formations, nodes, etc.
If you are past this stage and just want to control your breakouts, read on.
On store shelves there are a lot of products for home care for acne-prone skin. Every cosmetic company – no matter whether it is large, professional or “organic” – produces natural, organic products and has a special line for problem skin. Let's figure out how not to get lost in the variety of anti-acne products.
The four most common myths about the composition of cosmetic products:
Myth No. 1: Cosmetics are safe if they are labeled “non-comedogenic” or “non-acnegenic.”
The label “non-comedogenic” means that the product does not provoke the appearance of non-inflammatory open or closed comedones, known as blackheads and bumps/irregularities of the skin.
The term “comedogenicity” is not confirmed by law; it was invented by marketers to make cosmetic lines for minimizing and controlling acne seem reasonable, that is, to increase sales. But still, if a developer makes statements about the “non-comedogenicity” of his product, he is obliged to somehow confirm them.
In the best case scenario, the manufacturer tests its composition on the backs of volunteers whose skin is prone to clogged pores. If a cosmetic product does not increase the number of comedones, it is labeled as “non-comedogenic.”
For me, this is a very questionable study, primarily because the sebaceous glands of different locations have an unequal number of receptors that increase the production of sebum, which leads to comedones. Nevertheless, even such tests are still a plus, since an attempt is made to at least somehow substantiate the result. Basically, manufacturers simply quote the List of Non-Comedogenic Substances created by Dr. Kligman (who discovered cosmeceuticals for us) back in 1979, that is, there are no tests, just a naked theory.
The situation with tests for “acnegenicity” is approximately the same - they are very conditional.
Therefore, labels should not be trusted 100%. Myth No. 2. Mineral oil is comedogenic.
Many people believe that blackheads appear on them precisely because of the mineral oil included in the cosmetic product.
It is found in every second product, especially often in decorative cosmetics. Such statements are based on research from many years ago. Today there are many mineral oils: industrial - for lubricating mechanisms, cosmetic - the purest, without any impurities for cosmetics. And if the first can be comedogenic, then the second is not. Myth No. 3. Sunscreens - sunscreens - provoke acne.
This is almost true. Almost, because if inflammation appears 24–48 hours after applying the product, it is not acne, but irritation caused by sunscreen elements, mainly UV filters.
Acne is an immune response. And it takes weeks to trigger a response from the immune system.
Myth #4: Large pores associated with acne can be erased with makeup.
Only if you use so-called grouts - silicone-based products, which, when applied to enlarged pores, fill and smooth out all unevenness. The effect of the grout is purely visual and lasts until the first wash.
The size of the pores depends on the development and activity of the sebaceous glands: children do not have them, because the glands are not yet developed, but then what grows, grows. As you age, the activity of the glands decreases; after 60 years, your pores will be smaller.
Retinoids (substances analogues of vitamin A), which reduce sebum regulation, and regular cleansing, which pushes out sebaceous plugs, will help bring the pores to a natural state, but hoping to reduce their size is foolish.
Principles of self-diagnosis
We often tend to dramatize the situation and be too critical of our skin. A couple of pimples after fatty/sweet/salty foods or menstruation cannot even be called acne by any stretch of the imagination, especially with oily or combination skin types.
If you have fewer than 20 white-headed blackheads, fewer than 15 pustules, and fewer than 30 lesions in total, you have “mild” acne. Treatment usually takes up to 8 weeks with external remedies.
If you have 20 to 100 whiteheads, 15 to 50 inflamed bumps, and 30 to 125 breakouts in total, you have “moderate” acne. Treatment also takes several weeks and may briefly worsen during the process.
Moderate acne and more severe situations require consultation and professional treatment.
The dangers of self-medication
There is a misconception that as soon as a pimple appears, it is necessary to immediately bring down all the power of modern medicine and cosmetology on it: dry it, squeeze it, cauterize it, etc. In this case, it should go away immediately. Meanwhile, the inflammation that has been quietly smoldering inside the hair follicles or sebaceous glands for several weeks, until the increased sulfur content provoked it to come out, simply cannot take and go away in minutes.
Mechanical damage to the skin, rubbing with chlohexidine, lotions with dimexide, essential oils can lead to ulcers, burns, secondary infection and further aggravate the situation.
Just remember that to fight inflammation, it's better to underdo it than overdo it. When interfering with the body today, you need to think about what will happen to it tomorrow and in 20 years. For example, overuse of drying agents will lead to early wrinkles. It is important to accept that a 100% positive result is not possible if you are predisposed to acne due to genetic or other reasons. Your skin has already been repeatedly damaged at the level of the dermis and hypodermis and, most likely, inflammation will appear in these places. Just control it.
What else is worth paying attention to
There are three common additional causes of inflammation in acne-prone people. In order to level or minimize them, experts advise following certain recommendations.
Progesterone
If inflammation occurs in the second phase of the cycle, calm down, the condition of the skin worsens during this period, as the hormone progesterone works. Wait for the calm phase and carry out treatment. Don’t panic that your products don’t work; don’t rush to urgently buy something “more effective.”
Errors in diet
“Overdose of spices” or carbohydrates. Over the past few years, doctors and scientists have been inclined to believe that there is a connection between diet and acne, although this was previously denied. An imbalance of intestinal microflora increases the permeability of the intestinal walls; the amount of bacterial endotoxins (toxic substances) inhabiting the intestinal lumen increases in the blood, which leads to acne.
Drink tomato juice - it contains lycopene (affects sebum production), eat carrots - they are rich in carotenoids (prevent oxidative stress), pumpkin seeds - contain tryptophan (affects melatonin), sea fish - rich in omega acids (acne sufferers lack such acids), fermented milk products are a source of probiotic cultures that normalize intestinal microflora.
Indications
For each release form of Solcoseryl there are individual indications.
In the form of injections, the drug is prescribed when a patient is diagnosed with:
- occlusive peripheral artery disease grade 3 or 4;
- disturbances of venous blood flow with trophic lesions;
- strokes and traumatic brain injuries, which led to disruption of metabolic processes in the brain.
Ointment and gel for external use are used in complex treatment:
- minor abrasions and wounds;
- mild to moderate burns, frostbite;
- difficult-to-heal skin lesions: trophic ulcers, bedsores.
Ophthalmologists recommend the use of Solcoseryl eye gel to patients for the treatment of:
- injuries of the cornea and conjunctiva, their erosive lesions;
- scars after ophthalmological operations;
- eye burns of various types;
- dystrophic lesions of the cornea.
In addition, this gel is indicated for use in case of discomfort when wearing contact lenses and to reduce the time of getting used to them.
How to inject Solcoseryl for gastritis
Gastritis is a disease of the gastric mucosa that can occur for various reasons. Solcoseryl ampoules will not become the main drug used in the treatment of gastritis, but it can speed up the healing process, while the prescribed therapy will relieve the patient of the source of the problem.
The gastric mucosa can become inflamed not only as a result of poor nutrition, but also as a result of infection with gastrointestinal infections. The attending physician will first conduct an examination and evaluate the test results, which will allow him to prescribe effective therapy. Solcoseryl will be used as an addition to the main treatment, as it will help the stomach tissues to regenerate faster, ulcers to heal, and inflammation to disappear.
Side effects
The use of an injection solution in rare cases can lead to the development of allergic reactions, including anaphylactic shock. In this situation, you should immediately stop using the drug and prescribe symptomatic therapy in the form of antihistamines.
In addition, the process of performing the injection itself can be painful for the patient due to the potassium it contains.
When using the ointment, some patients may experience a burning sensation at the site of application.
Solcoseryl eye gel may cause short-term irritation, which is not an indication to discontinue treatment. The development of allergic reactions when using external forms of the drug is extremely rare.
Herpes “wakes up” when immunity decreases
Causes of recurrence of herpes on the lips: stress or emotional distress; various other diseases, in particular colds, flu, diabetes, HIV; poisoning or intoxication; drinking alcohol, caffeine and smoking; excessive ultraviolet radiation; hypothermia or overheating; onset of menstruation; overwork and exhaustion; poor nutrition/diet or stomach upset; other factors individual to each person.
After “awakening,” the virus travels back to the skin. As the virus moves through a nerve, it causes inflammation of the nerve tissue.
The development of herpes can be divided into several stages. At the first stage, the person feels unwell. At the site where the “fever” appears, there is pain, tingling, and the skin turns red. At the inflammation stage, a small painful blister filled with fluid forms. After some time, the bubble bursts and a colorless liquid containing billions of viral particles flows out of it. An ulcer appears in its place. At the final stage, the ulcer becomes covered with a crust.
Most often, herpes appears on the lips, but lesions can also appear on the face, in the ears or in the mouth.
Mode of application
Solution
Solcoseryl in the form of a solution is recommended to be administered intravenously slowly in the form of an injection or by drip, having previously diluted it with saline solution or 5% glucose solution. If intravenous administration is difficult, intramuscular injection is allowed.
For the treatment of venous insufficiency, the drug is prescribed for up to a month, combining it with the application of an external gel or ointment to the area of trophic ulcers.
Patients who have suffered a stroke are prescribed a course of treatment with Solcoseryl for 5 weeks. When treating traumatic brain injuries, short courses lasting 5 days are prescribed.
Ointment and gel
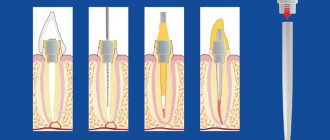
Ointment and gel for external use are applied directly to the wound. Before using them, the wound surface is thoroughly disinfected. In the presence of purulent discharge, surgical treatment may be required.
The gel is used to treat wet, fresh wound surfaces. When the affected area begins to epithelialize, granulation tissue appears and the wound dries out, you should switch to using Solcoseryl in the form of an ointment.
The course of treatment with external forms of the drug is carried out until the wound surface is completely healed and a scar is formed.
Ophthalmic gel
The eye gel is instilled into the conjunctival cavity 3-4 times a day, one drop at a time. In some cases, it is possible to use the drug hourly. The course of treatment lasts until complete recovery.
What is Solcoseryl ointment used for?
The drug is based on deproteinized dialysate obtained through special processing from the blood of calves. This substance is often used in medicine in countries such as China, Korea, and the entire CIS. It has proven itself to be an effective remedy that can:
- enrich tissue cells damaged due to hypoxia with oxygen and glucose;
- start tissue repair processes;
- activate healthy cell division processes;
- increases the level of energy produced by cells;
- protects the skin from external damage by forming a film on its surface;
- triggers the production of collagen by tissues.
Based on the activity of the drug, the drug can be used for:
- frostbite;
- psoriasis;
- anal ring cracks;
- cuts;
- abrasions;
- scratches;
- bedsores;
- acne marks;
- dermatitis;
First of all, to achieve the best effect, it is necessary to start therapy in the early stages of the problem.