Expecting a baby is one of the most wonderful periods in a woman’s life. Her thoughts are focused on dreams of the future baby and joyful worries about children's things, a stroller, and toys. But changes in the body sometimes prepare unpleasant surprises for the expectant mother. Thus, many women feel dryness, itching and burning in the intimate area during pregnancy. What caused them?
What should an effective disinfectant contain?
Today there are two types of antiseptics that work well against germs, bacteria, and viruses.
The first type is alcohol-based liquids; it should contain at least 60%, preferably more. If the content is less, then the protein shell of microbes and viruses will not be destroyed and some of them will remain invulnerable. The alcohol must be ethyl or isopropyl.
The second type of antiseptic is based on chlorhexidine. It does not erode longer, provides longer-lasting protection, but damages the skin of your hands. However, alcohol also dries the skin, so such liquids usually contain softeners.
Side effects
With long-term use of Chlorhexidine during pregnancy, there is a risk of developing negative manifestations:
- Temporary occurrence of enamel discolorations.
- Impaired taste perception due to the bitter taste of the drug.
- Dermatological reactions.
- Vaginal itching.
- The appearance of the symptom of “sticky palms”.
Cases of Chlorhexidine overdose do not occur in clinical practice, however, the solution should be used with caution by pregnant women who are hypersensitive to the active component due to the possible development of allergies.
How to protect the skin of your hands after using an antiseptic?
High-quality formulations already include various softeners, moisturizers, glycerin, and vitamins that reduce the effect of alcohol and chlorhexidine on the skin. However, sometimes this is not enough, especially with frequent use of solutions. To prevent irritation, redness, and allergic reactions, do not use too hot water for washing, use cream soap instead of regular soap, drink more water (7-8 glasses a day). If cracks and wounds appear, buy special ointments, do not delay treatment.
Indications and contraindications
The medication is often prescribed for various gynecological diseases:
- vulvovaginitis caused by microbes sensitive to the drug;
- for STIs, such as gonorrhea, syphilis, trichomoniasis, mycoplasmosis, genital herpes;
Chlorhexidine is also used in pre- and postpartum vaginal treatment, when treating the hands of medical workers before obstetric examination.
Chlorhexidine digluconate is often prescribed during pregnancy to rinse the mouth for dental problems:
- For diseases of the oral mucosa, including stomatitis of various etiologies, herpes, erosion, and candidiasis.
- In pathological processes affecting the gums - periodontal disease, gingivitis of pregnant women, periodontitis. Used in complex treatment.
- As prescribed by a dental surgeon after tooth extraction and other dental surgical interventions.
Chlorhexidine is widely used in the treatment of:
- tonsillitis;
- pharyngitis;
- laryngitis;
- tonsillitis.
The therapeutic effectiveness of eliminating these pathologies is achieved only with an integrated approach to the treatment of throat diseases, so it is important to adhere to the doctor’s recommendations. Carrying out inhalations or rinsing with Chlorhexidine without taking other medications may not lead to recovery, and sometimes even worsen the patient’s condition.
The solution has high activity against microorganisms, so Chlorhexidine can be used during pregnancy to treat many infectious diseases.
Contraindications:
- Individual intolerance.
- Dermatitis in various manifestations, since the drug can lead to aggravation of the disease.
- Doctors do not recommend using the drug simultaneously with other antiseptics.
- Chlorhexedine should not be used simultaneously with alkaline solutions and soap, as they neutralize its effect.
- Use with iodine-containing drugs is unacceptable due to their incompatibility.
Is it possible to drink antiseptic?
No you can not. Unfortunately, some people use antiseptics internally due to the presence of alcohol in the composition. The result of such use is burnt internal organs, severe poisoning, and this is at best; at worst, the person dies. For the production of antiseptics, two types of alcohol are used - ethanol and isopropyl. The second is cheaper, is not suitable for the production of alcohol-containing drinks due to toxicity and is not suitable for drinking, but due to its low price it is most often used in the manufacture of sanitizers.
Can Chlorhexidine be used during pregnancy?
The drug does not have a negative effect on the female body, and also does not penetrate the hematoplacental barrier, so the drug does not reach the baby. Therefore, the answer to the question whether it is possible to gargle with Chlorhexidine during pregnancy is obvious. Also, the substance does not pose a threat to the development of the embryo when used in the first trimester of gestation.
In addition to use for throat diseases, you can rinse the mouth with Chlorhexidine during pregnancy, and also use it for antiseptic treatment of the external genitalia.
Can alcohol be used as an antiseptic?
In its pure form, we do not recommend using alcohol as an antiseptic. In sanitizers, the amount of ethyl ranges from 60 to 80%; they are no longer used. The alcohol strength is 96%, meaning this concentration will almost certainly cause skin problems, especially with repeated use. In addition, even the simplest sanitizer contains auxiliary substances - glycerin, hydrogen peroxide and others. They not only perform antiviral functions, but also serve as softeners, humidifiers, etc. Thus, using alcohol carries the risk of burns, irritation, and other problems.
By the way, you cannot use vodka either, it is ineffective, since its strength is only 40%, which will not kill viruses.
Infections caused by antibiotic-resistant microflora represent an ever-growing threat in both hospital and community settings. Nosocomial infections lead to a decrease in the effectiveness of therapy, an increase in the duration of hospitalization and an increase in mortality.
Chlorhexidine bigluconate was developed in Great Britain in 1950. It is the first internationally recognized antiseptic for skin and wounds. One of the advantages of chlorhexidine, in addition to its pronounced antimicrobial effect, is its ability to bind to various biological substrates while maintaining its antibacterial activity, and then be slowly released, which leads to the preservation of effective concentrations of the drug. To date, there are no reports of resistance to chlorhexidine, despite more than 60 years of active use of the drug in the clinic. Chlorhexidine gluconate remains important in the prevention of nosocomial infections.
Widespread use of antiseptic methods for the prevention and treatment of infections followed the publication of Joseph Lister's The Antiseptic Principle in Surgical Practice in 1867. At the same time, “Lister’s antiseptics” met ardent opponents, whose main argument was the toxicity of the antiseptic they used (carbolic acid). Despite the availability of numerous antiseptics, the question of the safety and effectiveness of this group of drugs remains constantly relevant. The “longevity” of chlorhexidine and the prospects for its further use as one of the most powerful antiseptics widely used in clinical practice is a pressing issue for clinicians.
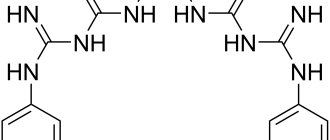
A cationic detergent (detergent), later named chlorhexidine, was synthesized during the development of antimalarial drugs in 1947. This compound has bactericidal antimicrobial activity, especially against gram-positive microorganisms. Of the 10,040 compounds, the first to enter the market was chlorhexidine gluconate, registered in 1954 by Imperial Chemical Industries Co.LTD (UK) as “Gibitan” - the first internationally recognized antiseptic for the treatment of wound surfaces and skin. In 1957, only 3 years after entering the market, the indications for its use were expanded to include not only skin treatment, but also use in ophthalmology, urology, gynecology and otorhinolaryngology. In 1959, chlorhexidine began to be used to control bacterial plaque, leading to its widespread use in dentistry. Currently, in clinical practice, chlorhexidine is preferred not only when treating the skin (hands, surgical field), but also as an oral antiseptic, including for the prevention of nosocomial infection. The most commonly used concentrations are 0.2% and 0.12% solutions. In addition to its effect on plaque and gum condition (gingivitis), chlorhexidine is effective in the prevention and treatment of caries, secondary infections after dental procedures or implant placement. Chlorhexidine reduces the bacterial load and the risk of bacteremia after dental procedures. It is also used in the treatment of recurrent atrophic stomatitis and stomatitis associated with the installation of dentures, primarily in groups of patients with orthodontic appliances and immune disorders. One of the main advantages of chlorhexidine, in addition to its powerful antimicrobial effect, is its ability to retain its antimicrobial activity when bound to various substrates. At the same time, it is released slowly while maintaining an effective concentration. This property is known as substantiveness. Chlorhexidine is not susceptible to blood, pus, or saliva. Chlorhexidine is pharmaceutically incompatible with soap and detergents (for example, those containing lauryl sulfate), alkalis and other anionic compounds (colloids, gum arabic, carboxymethylcellulose), and iodine. Compatible with ethyl alcohol, benzalkonium chloride (contained in contraceptives for local use Pharmatex and Benatex). Ethanol enhances the effectiveness of the drug. The bactericidal effect increases with increasing temperature. At temperatures above 100°C, the drug partially decomposes. Used in a neutral environment; at pH 5-8 the difference in activity is small; at pH above 8 it precipitates. The use of hard water reduces bactericidal properties. Compatible with drugs containing a cationic group (benzalkonium chloride, cetrimonium bromide).
The unique combination of properties of chlorhexidine also determines the variety of dosage forms.
Chlorhexidine is available in the following forms: • 20% concentrated solution – intended for dilution before use, used in medical institutions; • 0.05% solution in plastic and glass bottles of 70 and 100 ml - used without dilution, including at home; • Vaginal suppositories (suppositories) “Heksikon” containing 0.016 g of chlorhexidine, 1 or 10 suppositories in a package; • Vaginal suppositories (suppositories) “Heksikon D” containing 0.008 g of chlorhexidine – intended for children, 10 suppositories per package; • Gel containing 0.5% chlorhexidine. Chlorhexidine is included in the following preparations: • Solutions for mouth rinsing for dental diseases and manipulations (tooth extraction, opening of abscesses, professional cleaning, etc.) – Elgidium, Amident, Eludril; • Gels for gums, intended for the treatment of dental diseases and pain relief in the oral cavity (for example, when getting used to dentures), one of the components of which is chlorhexidine - Dicloran Denta, Elugel, Metrohex, Parodium, Elgifluor, Dentamet, Metrogyl Denta; • Elgidium toothpaste; • Solutions with other antiseptics – Baktoderm (with benzalkonium chloride), Chlorhexidine alcohol spray – for the treatment of skin infections, Citeal (with hexamidine and chlorocresol) – for topical use in gynecology, dermatology; • Ointments Bepanten plus and Depantol (with panthenol - wound healing effect), Bemilon (with betamethasone - anti-inflammatory effect); • Vaginal suppositories Depantol (with panthenol) – used in gynecology after surgical interventions; • Chlorhexidine in combination with lidocaine for local anesthetic action in the Lidocaine-Asept spray and Instillagel and Kategel gels with lidocaine; • Lozenges for sore throat, stomatitis and other diseases of the oropharynx and oral cavity – Hexoral tabs, Anti-Angin formula, Sebidin.
Groups of inhalation drugs:
- Antiseptics (Furacilin, Dioxidin, Miramistin)
- Antibiotics (Gentamicin, Tobramycin)
- Anesthetics (Lidocaine)
- Hormonal drugs (Cromohexal, Budesonite, Pulmicort, Dexamethasone)
- Immunomodulators (Interferon, Derinat)
- Mucolytics (Fluimucil, Lazolvan, Ambroxol, Ambrohexal, Pulmozyme, Acetylcysteine)
- Bronchodilators (Berodual, Fenoterol, Ventolin, Berotek, Salamol)
- Herbal medicine (Rotokan, Tussamag, Chlorophyllipt)
- Vasoconstrictors (Adrenaline, Naphthyzin)
- Alkaline and saline solutions (0.9% saline)
Hygiene after childbirth
It is generally accepted that the postpartum period lasts about 6-8 weeks, until all organs and systems of the body return to their previous state. After childbirth, a woman is very vulnerable to infections, because the cervix remains open for a long time, and the internal genital organs sometimes appear as one large wound.
The baby, in turn, is also very vulnerable to infections at first. In order to avoid various kinds of complications, it is very important for mom to follow the rules of intimate hygiene.
General recommendations:
- wash your hands often, they should always be clean;
- instead of washing your hands with soap, use sterilliums more often - antiseptic gels or balms (unlike soap, they actually destroy 99% of bacteria, and good sterilliums also maintain the Ph factor of the skin);
- take a shower at least twice a day;
- change your shirt every day to a clean one;
- towels for hands, mammary glands and intimate hygiene must be strictly individual, washed at 90 degrees and ironed with a hot iron on both sides;
- go to the toilet every 3-4 hours, even if you don’t feel the urge (sensation after childbirth may be temporarily absent, and signals to the brain about the fullness of the bladder or rectum may not be received);
wash yourself after each toilet (do it with a clean hand, from front to back);- After washing, the skin of the perineum should be dried by blotting a clean towel or diaper;
- do not take a bath or visit the sauna in the first 2-3 weeks after birth;
- in case of exacerbation of hemorrhoids after childbirth, you should not use toilet paper after visiting the toilet, it is better to simply wash yourself with lukewarm water;
- if you received stitches after childbirth, try not to touch them with your hands at first, and when washing, simply direct a weak stream of water to the area of the stitches; also be sure to undergo antiseptic procedures for stitches;
- Do not douche under any circumstances during the postpartum period without a doctor’s recommendation, as this may cause a decrease in local protection and increase the likelihood of infection.
Lingerie
The following basic requirements apply to underwear during the postpartum period:
it should allow air to pass through well (preferably it should be made of natural fabrics, not synthetics); do not adhere too tightly to the skin, especially the genital organs, and do not create a “greenhouse effect”, do not injure, especially the seams; underwear should be comfortable and not restrict movement.
There are now disposable underwear on sale that are specially designed for use during the postpartum period. Most often, maternity hospitals are prohibited from bringing your own underwear - only disposable underwear is allowed.
Linen change frequency:
- the shirt must be changed daily;
- We change panties once a day or even more often;
- bra at least once every 3-5 days;
- change bra pads as they get wet so you don’t have to change your bra every day;
- It is better to change bed linen at least once a week or use special disposable linen for the postpartum period;
- The diaper, which is laid on top of the sheet in the maternity hospital, is changed daily.
Sanitary napkin
If the use of pads is allowed in the maternity hospital (some maternity hospitals do not allow the use of pads in the first days after birth, but only loose underwear to hold the diaper in place), use highly absorbent pads or buy special postpartum pads. They should be changed as they become saturated with secretions, at least once every 4 hours. Ideally after every visit to the toilet. It is especially important to follow this rule in the first days after childbirth, while lochia comes out (they are a very good breeding ground for bacteria). If pads are not allowed in the maternity hospital, then, apparently, you will be given special diapers. This is done so that the doctor can easily determine the condition of the woman in labor by the nature of the discharge.
Intimate hygiene products
The following basic requirements apply to intimate hygiene products during the postpartum period:
- good skin cleansing, without irritation;
- absence of allergic reactions;
- antibacterial and anti-inflammatory protection;
- neutral PH factor.
Baby soap or soap with an antibacterial effect may be perfect for these purposes. Special products for intimate hygiene are also suitable. It is better to check their effects on the skin before giving birth to prevent an allergic reaction to them.
Important! Do not use household soaps for intimate hygiene.
Breast care
It is not at all necessary to wash your breasts too often, maximum 1-2 times a day, otherwise the protective layer of the nipples will suffer greatly and they will crack. Wash your breasts with your hands without washcloths or sponges.
Before and after feeding, express a few drops of milk, this is a good prevention of cracked nipples. After lubricating the nipple with milk after feeding, let it dry a little in the open air. In addition, for cracks in the delicate skin of the nipples, use creams that your doctor recommends.
Mother’s hygiene procedures during and after childbirth occupy a significant part of the day. The child’s hygiene procedures are even more important. But these are necessary conditions for raising a healthy and strong baby. Therefore, be prepared for this and do not neglect them.
What you need for the rinsing procedure
To rinse your nose correctly, you need to prepare certain devices. Everything you need is freely available on pharmacy counters.
For processing, you will need a syringe without a needle (5 ml is enough) or a syringe bulb (no more than 50 ml). It is convenient to use Chlorhexidine solution with a special “neti pot” washing device made of ceramic or plastic. The choice of equipment depends on preference.
Chlorhexidine is collected in a container and rinsing begins. It is advisable to do this in the bathroom, or above the basin. The person leans forward 45 degrees, his head is turned slightly to the side. Mouth breathing is smooth and constant. The contents of the container are slowly poured into one nostril. With the correct position of the body, the liquid will pass through the nasal passage and pour out through the second nostril or mouth. There should be no discomfort, burning or itching. Daily rinsing of the sinuses helps to quickly get rid of the infection. Eliminates runny nose, improves overall health.
—>
Pediatricians do not recommend clearing the nose of infants with antiseptic. Young children have narrow airways. Under high pressure, Chlorhexidine can get into the child’s ears, thereby triggering the development of otitis media. In this case, self-medication is completely contraindicated. Any actions must be agreed with the attending physician, and therapy is carried out only under the supervision of a specialist.
- How to gargle with Chlorhexidine for adults, children and pregnant women?
Children over 6 years old wash their noses like adults. To prepare the child physically and psychologically, doctors recommend that parents show the procedure by example.