Home → Articles → Recommendations after gum surgery
The dental team at the Stomatolog 11 clinic strongly advises that you follow all recommendations after gum surgery. Safe dental treatment using modern dental devices in the clinic creates conditions for a comfortable postoperative period. Maintain your oral health after surgery by following the tips below.
Sign up for a consultation at the dental clinic “Stomatolog11” in the Northern Administrative District:
Make an appointment
Contraindications
Dissection of soft tissues with further installation of drainage is not possible in all cases. Among the prohibitions to the procedure are:
- pathologies associated with blood clotting disorders;
- allergy to painkillers used before the procedure.
In the latter case, the doctor must select a drug that does not cause adverse reactions in the patient. There are no other contraindications to drainage. If the cheek is swollen, and necrotic masses have accumulated in the periodontal tissues, then the easiest way to deal with the problem is by installing drainage.
Why install drainage?
In dentistry, drainage is used in the following cases:
- for tissue healing after removal of a problematic tooth;
- with alveolitis;
- after opening the flux;
- when an abscess or cyst forms;
- for administering medications directly into the wound.
The patient should not worry if his gums were cut and a drainage system was installed. Drainage is used to remove purulent exudate and ichor. If drainage is not installed, the opened source of infection will heal quite quickly after cleansing, but if the inflammatory process is not stopped, the formation of purulent masses will begin again. In this case, a new operation will inevitably be required.
Indications
Normally, local mucosal immunity is able to protect the wound from infection. Saliva contains a natural antibiotic - lysozyme, which destroys pathogenic microorganisms. Thus, the wound cleanses itself. But there are situations in which local protection weakens and there is a risk of complications.
Rinsing after tooth extraction is indicated in the following cases:
- Inflammation (pulpitis, periodontitis) appeared before the operation.
- The gums were opened and there was additional trauma. For example, if there was flux and drainage was installed.
- There are untreated inflammatory diseases in the oral cavity: stomatitis, carious teeth, tartar.
In these conditions, there is a high risk of infection of a fresh wound. In these cases, rinsing is needed to disinfect, destroy bacteria, and reduce the risk of complications. Often in such cases, additional oral medications are prescribed: antibiotics and anti-inflammatory non-steroidal drugs.
The gum has moved away from the tooth: treatment
If the gum has moved away from the tooth, treatment will largely depend on the severity of the inflammation. For example, if a patient seeks help at a fairly early stage of inflammation (when the depth of periodontal pockets does not yet reach 3 mm and there is no tooth mobility), significant success can be achieved in the treatment of periodontitis and the process can be completely stopped. Advanced cases of gum inflammation will require much more complex treatment and serious financial costs. Next we list the main stages of treatment.
1) Consultation and x-ray diagnostics –
It is necessary to begin treatment with a consultation with a periodontist and a panoramic photograph of the teeth, which will allow you to create an optimal treatment plan taking into account the condition of your teeth and gums. The image will allow you to determine the amount of destruction of bone tissue around each tooth, the location and depth of periodontal pockets, and will help guide the patient in the need for splinting of mobile teeth, the need for prosthetic replacement of missing teeth, and make the correct diagnosis.
An example of a panoramic image of a patient with periodontitis –
Looking closely at the image, you may notice that the level of bone tissue (the bone looks in the image as fine-mesh looped tissue and normally should reach the necks of the teeth) is reduced in different teeth by 1/4 to 4/5 of the length of their roots. The patient has decayed teeth that need to be removed, as well as carious teeth that require treatment (24stoma.ru). The level of bone tissue is most reduced in the front teeth of the upper and lower jaw, which in this case was the result of not only inflammation of the gums, but also the absence of the chewing group of teeth.
To treat gums, it is best to contact not ordinary dental therapists or hygienists, but periodontists. These are the dentists who specialize in gum treatment. The first and most important stage of treatment will be ultrasonic teeth cleaning. Next, a course of anti-inflammatory therapy is carried out, which in most cases can be successfully carried out at home.
2) Removal of dental plaque –
First of all, it is necessary to remove the cause of inflammation - microbial plaque and dental deposits. They are removed from the teeth using an ultrasonic scaler (Fig. 15), usually over several visits. It is simply impossible to remove all dental deposits in just 1 visit in a patient with periodontitis, because... It takes a lot of time to remove subgingival dental plaque, which is localized in periodontal pockets below the gum level.
It is subgingival dental plaque that poses the main danger for further progression of inflammation, so sometimes it is necessary to prescribe the patient even 3-5 times. Learn that without professional cleaning, all other stages (for example, anti-inflammatory therapy, splinting) will be completely meaningless.
Most dentists and hygienists won't bother with finding and removing subgingival calculus...as experience has shown. Therefore, it is very important to find a competent specialist. Anti-inflammatory therapy is prescribed immediately after 1 session of removing tartar, and within the first 24 hours you will be able to notice changes in the appearance of the gums. In parallel with the reduction in gum swelling, their volume will also decrease, which will allow you to see new portions of dental plaque and remove them during subsequent visits.
Removing dental plaque with ultrasound: video
You can see in the following photos what happens when subgingival tartar is removed poorly. The first photograph shows that the gums are visually in good condition, although a periodontal probe revealed the presence of a periodontal pocket about 5 mm deep. The second photograph was taken after the gums were detached from the teeth, and it shows a very large amount of destruction of bone tissue, which arose due to the presence of small subgingival tartar on the surface of the tooth root.
3) Anti-inflammatory therapy –
The course of anti-inflammatory therapy usually lasts 10 days. In most cases, it is carried out by the patient himself at home, after doctor’s prescriptions and patient education. However, if the patient has deep periodontal pockets with purulent discharge, the doctor may additionally prescribe washing the periodontal pockets, which is done using a syringe and antiseptic solutions. In some cases, antibiotic therapy may also be prescribed for periodontitis.
Anti-inflammatory treatment regimen - usually a complex is prescribed, consisting of an antiseptic mouth rinse and application of gel to the gums. The procedures are carried out 2 times a day (morning and evening, after meals and subsequent oral hygiene), for 10 days. Most often, a complex of the following drugs is prescribed:
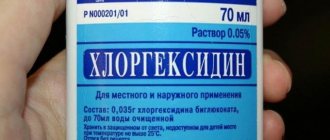
- rinsing with Chlorhexidine (instructions)
- “Cholisal-gel” applications (instructions)
In patients with periodontitis, the correct choice of treatment agents is very important. For example, a standard 0.05% solution of chlorhexidine, sold in pharmacies for 40 rubles, is advisable to use only for superficial inflammation of the gums (gingivitis), but for periodontitis it is better to use a 0.2-0.25% concentration of this antiseptic. It is a big plus when such a solution contains not only a good concentration of chlorhexidine, but also other active ingredients (for example, aluminum lactate for bleeding gums or extracts of medicinal plants).
Antiseptic mouth rinse is carried out after breakfast and oral hygiene, rinse your mouth for 1 minute. After this, the gums need to be dried with a dry gauze pad to remove excess saliva, and an anti-inflammatory gel should be applied to the gum edge. The gel is applied in front of a mirror using a finger, and usually only on the front side of the teeth. After such treatment, it is not recommended to eat for 2-3 hours, and also not to drink for 30 minutes. There are a lot of remedies for treating gums, and we hope that our next articles will help you understand their diversity -
→ The best antiseptics for mouth rinsing, → Rating of the best gels for treating gums.
4) Oral hygiene training –
If you have not yet forgotten the beginning of the article, then remember that the cause of periodontitis and destruction of the dental-gingival attachment is unsatisfactory oral hygiene, which leads to the accumulation of microbial plaque and tartar on the teeth. Therefore, in addition to the basic treatment that we described above, it is very important to constantly maintain high-quality oral hygiene.
Good hygiene doesn't mean just brushing your teeth twice a day, that's not enough. Good oral hygiene includes brushing your teeth after every meal, not snacking on cookies or candy between meals, and regularly using dental floss. You can read about absolutely all the recommendations in the article at the link above. Below, you can watch the video on how to properly use a toothbrush and dental floss.
How to use dental floss and brush correctly -
In the presence of periodontal pockets and mobile gingival margins, it is important to carry out hygiene below the gum level. This can be done using special devices - home irrigators. Special attachments allow you to rinse at home not only areas of the oral cavity that are difficult to reach for hygiene, but also periodontal pockets below the level of the gingival margin. Irrigators can use both ordinary boiled water and special medicinal solutions.
Something went wrong…
What should you do if your gums, which are supposed to heal after surgery, still hurt terribly? The problem may be with the neighboring tooth. A wisdom tooth grows crookedly, touches a neighbor as it grows, and can damage its enamel so that the neighbor will develop caries. In this case, the only correct solution is to remove the “eight”, but this is a complex operation that will require a strong painkiller.
After the operation, the following complications occur:
- When the gum is cut, it often swells. In other cases, the tumor becomes so large that the cheek swells. This is a symptom of alveolitis of the socket - a common disease that occurs due to an infection in the wound. Gum healing stops. Alveolitis is a simple disease, but it brings its share of discomfort and pain. If you notice its symptoms, do not delay it any longer, consult a doctor.
- Sometimes heavy bleeding begins after surgery: due to blood pressure or damage to a vessel. Did the bleeding start at home? Fold the swab and apply it to the wound or apply some ice to your cheek. Does the bleeding persist over time? Call an ambulance, you can't handle this on your own.
- High temperature indicates inflammatory processes. Take antibiotics as directed by your doctor.
- After surgery, the patient is often tormented by painful sensations. Severe toothache is relieved with painkillers as prescribed by the dentist.
Suction drainage from the pleural cavity
Suction tube
For suction drainage of the pleural cavity, various rubber and synthetic tubes are used.
For the most commonly used drainage, a rubber tube about 40 cm long with several side holes at the end is used. This tube is placed along the lung (from the base to the apex) and passed over the diaphragm from the pleural cavity to the outside. The drainage is attached to the skin with a knotted U-shaped suture. When the suction drain is removed, the threads are tied again, thereby sealing the hole in the chest. A three-barrel suction catheter (Viereck) is advantageous, allowing free passage of the tube inserted inside.
Insertion of suction drainage
In the chest between the two pleural layers, the intrapleural pressure is lower than atmospheric pressure. If air or liquid gets between the pleural layers, then the normal physiological state can only be restored by long-term suction drainage. A closed drainage system is used to suction pleural fluid for recurrent pneumothorax and to treat empyema. This drainage is now usually inserted into the intercostal space through a trocar. The thickness of the drainage tube is determined in accordance with the consistency of the substance being sucked out (air, as well as watery fluid or serous, fibrinous, bloody, purulent fluid).
On the drainage, mark with paint or thread the place to which it will be inserted. The size of the trocar must correspond to the size of the drainage. It is advisable to have at least three trocars of different sizes with suitable tubes of 5, 8 and 12 mm in diameter. Before inserting the trocar, you must make sure that the selected drainage tube passes through it easily.
The site of the skin incision is filtered with novocaine to the pleura. A test puncture in the designated area makes sure that the desired air or liquid is really there. The assistant gives the patient the necessary position: the patient must sit and lean on the highly raised operating table so that the puncture area protrudes as much as possible, and the selected intercostal space is, if possible, expanded. A scalpel is used to cut the skin over an area slightly larger than the size of the trocar. Then the trocar is inserted with a strong movement along the upper edge of the rib into the pleural cavity. After removal of the trocar, unimpeded release of fluid or free entry and exit of air indicates its correct insertion. Drainage is performed and the trocar tube is removed. If you are not convinced that the drainage is in the right place, you should, in order to prevent the trocar from puncturing the lung, heart or large vessel, perform the puncture again, taking all measures to localize it under X-ray control.
Before closing each thoracotomy hole, a drainage is introduced into the pleural cavity, which is brought out above the diaphragm through a separate hole in the intercostal space. Through a hole measuring about 1-2 cm, a forceps is inserted into the pleural cavity under the control of the eyes and under the protection of the left hand to ensure the correct position of the drainage from the inside. The drainage is pulled through the chest wall with a forceps from the inside to the outside. Pay attention to the fact that the drainage section, free from holes, is at least 5 cm in the chest cavity. If the fixation of the drainage to the skin is broken, then it slips out, and the first side hole appears outside the pleural cavity above the skin. In this case, the closed system turns into an open one, suction becomes ineffective, and pneumothorax often occurs.
Suction systems
There are so-called individual (“bed side”) and centralized suction systems. The suction action due to the hydrostatic effect can be obtained by a tube lowered under water, a water or gas pumping device (in this case the action is based on the valve effect) or an electric pump. Both individual and central systems must ensure individual regulation. If the release of air from the lung is insignificant, then due to its simplicity, the Biilau drainage system is still successfully used today, which can be sufficient to straighten the lung. A glass tube immersed under water (disinfectant solution) is equipped with a valve made from a finger cut off from a rubber glove, which protects against reverse suction. The Biilau system uses the physical law of communicating vessels to move bottles under the bed to create a suction effect.
The Fricar air pump best meets modern requirements. This device can work for many days without interruption and without heating up. The strength of the suction effect can be precisely adjusted.
Central suction devices are triggered by an oxygen canister system or a powerful suction pump. The system of outgoing tubes, if necessary, supplies hospital departments located on different floors. Depending on the need, the required number of hospital beds can be connected. An oxygen-powered system has the advantage that the suction and supply of oxygen to individual hospital beds is provided by the same tubing system. The suction effect is provided by a valve tube mounted along the oxygen flow. In this case, however, the effect produced by the central suction pump is not achieved.
Individual adjustment can be carried out using a dosimeter tap connected to a well-functioning pressure gauge, or through the so-called. three bottle system. The latter can be easily prepared by yourself. This system also has the advantage that it can easily and reliably create a very low suction effect (from 10 to 20 cm of water column). It is rarely possible to achieve such low pressure values using factory pressure gauges.
Indications for suction drainage
Spontaneous and traumatic pneumothorax, hemothorax
Spontaneous pneumothorax occurs at a young age, more often as a result of rupture of single pulmonary alveoli in the apex of the lung, in older people - as a consequence of rupture of alveolar vesicles with diffuse emphysema. Due to the fact that the number of patients with emphysema is constantly increasing, the number of cases of spontaneous pneumothorax is becoming more frequent. The same applies to traffic accidents that result in closed injuries in the chest cavity, which often occur with pneumothorax or hemothorax.
Correctly performed pleural puncture for spontaneous pneumothorax is practically safe, and its benefits can hardly be disputed. If the flow of air from the damaged lung is completely stopped and the perforation site is closed, then it may be possible to completely remove the air that created the pneumothorax with a simple closed puncture. If pneumothorax recurs after puncture (even repeated), then drainage with long-term suction should be used. Recurrence of pneumothorax, even after prolonged drainage with suction, can only be reliably eliminated by surgery.
Traumatic pneumothorax most often results from rib fractures. When a rib fragment injures the lung, most often a significant amount of air comes out of it, and a tension pneumothorax occurs. At the same time, subcutaneous or even mediastinal emphysema may occur. Spontaneous pneumothorax can also occur when the pulmonary alveoli rupture or due to blunt force on an emphysematous lung. Therefore, in patients with pulmonary emphysema, chest injuries are often associated with the occurrence of pneumothorax, often severe tension pneumothorax. The principles of treatment for spontaneous and traumatic pneumothorax are the same.
If clinical symptoms indicate tension pneumothorax (severe respiratory failure, subcutaneous emphysema, mediastinal shift), then drainage of the pleural cavity should be performed immediately. If these symptoms are not present, then a closed puncture is performed and the air is sucked out. After this, the needle is left inserted into the pleural cavity, and its nozzle is connected to a pressure gauge and the pressure in the pleural cavity is determined (whether it is higher or lower than atmospheric). If the pressure in the pleural cavity is indicated by the pressure gauge needle in the positive direction, it means that air continues to be released into the pleural cavity, and, therefore, drainage is necessary. This issue can, of course, be resolved by X-ray examination. If there is a total pneumothorax, then drains are inserted in two different places. One of them runs along the posterior axillary line above the diaphragm in the VII-VIII intercostal space, the other is inserted along the midclavicular line between the 1st and 2nd ribs. In our experience, drainage inserted under the collarbone performs the task of straightening the apex of the lung better.
In case of encapsulated limited pneumothorax, drainage should be inserted locally, under X-ray control after a test puncture.
Empyema of the pleura
Pleural empyema is a disease for which treatment with suction from the pleural cavity is absolutely indicated.
The principle of treatment of empyema does not depend on the causative agent of the disease. It consists of gluing the pleural layers and eliminating the empyema cavity through early drainage and suction of fluid. Treatment with suction from the pleural cavity is combined with targeted local chemotherapy, based on the identification of the pathogen and its resistance to the drugs used. Most empyemas result from infection of the exudate. In this case, incorrect and insufficient suction from the pleural cavity plays a certain role. In cases where pockets with delimited fluid form in the pleural cavity, their complete emptying becomes increasingly difficult, more difficult, and infection is more likely. In such cases, complete recovery can only be ensured by surgery.
Suction treatment may fail for two reasons: one is the presence of pleural cords, the other is a bronchopleural fistula.
Pleural moorings are often the result of insufficient emptying of the pleural cavity. When moorings have already formed in the pleural cavity and the walls of the empyema cavity are thickened, there is little chance of eliminating the empyema by suctioning out the fluid. The ability to expand the lung in this case is also very controversial. In this case, drainage with suction is a preparatory measure before the inevitable operation. Radical surgery (decortication) is performed only after the patient’s general condition has improved by washing the pleural cavity and targeted antibiotic therapy.
Bronchopleural fistula reduces the effectiveness of suction and thereby the prospect of lung expansion. In cases where there is a large bronchial fistula and its closure is contraindicated (for example, a rupture of the cavity, tumor disintegration, rupture of a cystic, emphysematous lung that has lost its elasticity), success cannot be expected from the use of suction. On the other hand, suction can also be used in cases where surgery is indicated. In elderly patients, with low general resistance and the possibility of severe complications, surgery becomes impossible. Then all that remains is to leave the patient with permanent drainage.
In case of chronic pleural empyema, drainage should be inserted into the pleural cavity at its lowest point. Large-diameter drains are used so that the thick liquid does not close the lumen and it is easy to wash the pleural cavity. Often, in the area where the drainage will be introduced, a rib resection (2-3 cm) is performed.
Postoperative suction from the pleural cavity
In order to remove fluid that accumulates after thoracotomy from the pleural cavity and maintain normal intrapleural pressure, a suction drain should be available.
If during pleural operations and mediastinal, transthoracic interventions on the esophagus, stomach, heart and large vessels there was no damage to the lung, then the chest can be closed with the introduction of one perforated drainage into the pleural cavity. Drainage is carried out above the diaphragm along the midaxillary line with its pleural end installed at the level of the apex of the lung.
Two drains are inserted into the pleural cavity if the lung was damaged during separation of adhesions, as well as after resection or excision of lung tissue. In such cases, one of the drains is inserted along the anterior and the second along the posterior axillary line. The use of a third drainage may be considered relatively appropriate when it is brought to the site of anastomosis of the esophagus or bronchus or when thoracoplasty is performed in combination with lung resection (for suction from the subscapular space).
After removing the lung, one drain with a diameter of 12-15 mm is inserted into the pleural cavity and placed in the lower part of the cavity so that a piece of drainage 10-12 cm long is equipped with 2-3 side holes. Active suction through this drain is prohibited.
After median sternotomy, a drainage is inserted retrosternally and its second end is brought out in the epigastrium.
Intensity and duration of suction
The intensity of suction through drainage from the pleural cavity depends on the cause of the disease, the condition of the lung and the nature of the operation. The flow of air from the lung into the pleural cavity is of decisive importance. If this occurs, then more air should be sucked out of the pleural cavity per unit time than is supplied there. Only in this way can gluing of the pleural layers be achieved. In practice, however, this is often not feasible. If the connection of the bronchus with the pleural cavity is significant (for example, in the case of a bronchial fistula), then intensive suction cannot achieve the goal. If you increase the suction force, then at the same time the patient will experience increased respiratory failure due to “air theft” from the tidal volume. Despite this, the lung will not be able to expand. In such cases, surgery is inevitable.
When the lung is damaged or after lung surgery, air most often escapes from a hole the size of a pinprick. In this case, specialized suction is indicated. In children and adolescents, due to the fact that their lung parenchyma is healthy and not affected by fibrosis and emphysema, it does not matter with what force the suction is performed. It doesn’t matter whether they suction with an intensity of 25 cm of water. Art. or simple underwater drainage, the lung will expand in 24-48 hours. The drainage can be removed after 48-72 hours. This is the advantage of elastic tissue capable of lung retraction in young patients. With emphysematous lung in an elderly person, the situation is different. The pinprick holes become gaping holes in the lung because the surrounding tissue is unable to contract. If you try to reduce the flow of air coming from the damaged lung by increasing the intensity of suction, you can easily get a paradoxical effect. The flow of air from the lung will increase. Small holes, due to prolonged suction, stabilize and turn into fistulas.
What to do in such cases? Begin gentle suction from the pleural cavity (5-6 cm of water column) and pay attention to ensure that tension pneumothorax does not occur. Thanks to this, the resulting fibrin seals small holes in the lung. Within 24 hours, a decrease in the release of air from the damaged lung begins to be detected. The intensity of suction can be increased slightly. On the fourth day you can already suction with an intensity of 10 cm of water. Art., if no unforeseen complications arise, then the drainage can be removed on day 4-5.
The same principles are followed when treating spontaneous and traumatic pneumothorax with suction.
If there is a significant intake of air from the emphysematous lung, they begin to carefully perform suction with a gradual increase in its intensity. If, after many days of treatment with suction, the release of air from the lung does not stop, then it is recommended to immediately undertake surgery, without waiting for the development of infection in the pleural cavity. If suction from the pleural cavity continues for more than a week, the development of infection becomes real.
In cases where the patient does not undergo surgery due to low general resistance, suction from the pleural cavity remains to be continued. Prolonged and specialized suction under the guise of drug treatment may be more or less effective. The pleural layers are glued together completely or partially. Only small limited cavities remain that do not lead to complications. The drain can be removed.
In the treatment of pleural empyema, long-term use of suction drainage is a common method. The empyema cavity gradually becomes smaller and smaller, the amount of fluid decreases, and in the end it can become bacteriologically sterile. If the daily amount of fluid extracted from the pleural cavity does not exceed 10-15 ml, then the suction is stopped, the drainage is shortened, but left until the residual cavity is completely closed.
In what cases is drainage installed on the gum?
There are many pathologies in dentistry for which drainage is installed on the gums. These include:
- flux - is a manifestation of periodontitis and is accompanied by severe swelling of tissues
- neoplasms in the roots of teeth - drainage is installed on the gums if abscesses and cysts are diagnosed
- alveolitis - inflammation of the tooth socket
- in order to accelerate the healing of the wound surface after complex tooth extraction
- if necessary, regularly inject medications into the lesion
Gum drainage, photos of which you can see on thematic websites, plays a significant role in dentistry. It ensures the removal of pathological fluids and access of drugs even into the deep periodontal tissues.
There are few contraindications to drainage. The procedure cannot be performed if you are allergic to the anesthetics used during the procedure or have a blood clotting disorder.
How long should drainage remain in the gum?
Patients are most concerned about the question: how long should drainage remain in the gum? This period is determined individually depending on how quickly the swelling of the periodontal tissue subsides. It is the disappearance of this symptom that indicates complete cleaning of the wound and the beginning of its healing.
Only a doctor can determine exactly when to remove the drainage from the gums, taking into account the nature of the pathology. As a rule, the wearing period is 4-5 days. This is enough to clean the wound from pathological fluids. Sometimes the drainage falls out earlier, but complications are not observed - this means that the wound cleared earlier.
Stages of drainage
The procedure can only be performed by a specialist. Trimming the gums and installing a rubber tube occurs in several stages:
- Examination of the oral cavity by a dentist.
- Taking an x-ray to determine the depth of the tumor and the extent of its spread to adjacent tissues.
- Injection of an anesthetic into the problem area. Does it hurt to cut your gum? The procedure is accompanied by significant discomfort, so anesthesia is used to minimize pain.
- Resection of the seal using a scalpel.
- Cleaning the purulent cavity using antiseptic agents.
- Fixation of a rubber tube to drain pus.
Using an X-ray of the oral cavity, the doctor can examine the condition of the roots of the teeth and, if necessary, prescribe extraction of problematic units
In severe cases, the drainage is left in the oral cavity for 3-5 days, until the swelling subsides and the ichor stops oozing from the wound. The drain may fall out on its own or be removed by a doctor. If swelling and inflammation persist 5 days after the intervention, you should immediately contact your dentist.
How to rinse your mouth after tooth extraction: list of products
There are several groups of drugs for sanitation of the mouth after dental surgery. Some kill the infection, others promote the restoration of the mucous membrane. How to rinse your mouth after tooth extraction in your particular case will be determined by your dental surgeon. Don't make your own appointments.
When choosing a medicine, the doctor evaluates several factors:
- condition of the wound;
- complexity of the operation;
- patient's age;
- individual intolerance to some components.
Let us briefly look at the most effective and popular solutions in dentistry.
Miramistin is a leader among antiseptics with a wide range of applications. Acts against infections of bacterial, fungal and viral nature. The product is produced in the form of a solution and an aerosol. The concentration of the active component is 0.01%. Usually 3-4 rinses are prescribed per day for up to a week. The medicine can be used at any age, during pregnancy and breastfeeding.
Chlorhexidine is the next most effective antiseptic drug. Disinfects wounds from bacteria, some viruses and protozoa. For dental procedures, a 0.05% solution is used. Prescribed in the form of baths and rinses three times a day. A huge advantage of chlorhexidine is its prolonged action: the antiseptic effect remains for another four hours after use.
Furacilin is a long-known strong antibiotic. In addition to disinfection, furatsilin also promotes wound healing. The medicine is released in tablet form. You need to prepare the solution yourself by mixing 1 tablet in 100 ml of saline solution. Rinse the wound 3-4 times a day for 5-6 days.
Chlorophyllipt is a disinfectant solution that is especially harmful to staphylococci. Works great in patients with concomitant chronic tonsillitis and pharyngitis, as they are most often caused by staphylococcus. The course of treatment is prescribed individually.
Traditional medicine recipes do not lose their relevance. Properly prepared decoctions and infusions of medicinal herbs are useful: chamomile, calendula, oak bark, sage, St. John's wort.
But what doctors do not recommend are solutions that contain salt, iodine, brilliant green, and potassium permanganate. These components have an irritating effect on the diseased mucous membrane and can cause a chemical burn.
Why does the gum move away from the tooth?
A prerequisite for the destruction of the periodontal attachment is the presence around the necks of the teeth - soft microbial plaque or supragingival tartar. The formation of dental plaque occurs due to irregular oral hygiene. In some patients with periodontitis, tartar may not be visually visible, because... when the attachment of the gum to the tooth is destroyed, it can already be localized below the level of the gum (then it is called “subgingival”).
But usually the destruction of the attachment of the gums to the teeth is always preceded by a long period of chronic inflammation of the gums, during which the patient is only bothered by periodic bleeding of the gums, possibly bad breath, redness or cyanosis of the gingival margin, as well as swelling of the gingival papillae. These symptoms are characteristic of gingivitis, an inflammatory disease of the gums in which the attachment of the gum to the tooth is not yet broken.
The lack of professional treatment for gingivitis (usually patients during this period self-medicate using antiseptic rinses and toothpastes for bleeding gums) leads to destruction of the attachment of the gums to the teeth. As a result, so-called periodontal pockets (gingival pockets) are formed between the teeth and gums, and patients in this case may complain that their gums have moved away from their teeth.
Stages of gum inflammation (gingivitis and periodontitis) –
Conclusions: Figure 10 shows the differences between gingivitis and periodontitis, and that with periodontitis, the gums are not attached to the teeth to the full depth of the periodontal pockets (from 3 to 6 mm or more). Therefore, if your gum has moved away from a tooth, there is simply no point in delaying a visit to the dentist, unless, of course, your goal is to remove these teeth in the near future. And in this case, there is no method of self-medication (magic rinses or ointments for gums) that would allow you to save the situation without going to the dentist.
In the absence of professional treatment of gums by a dentist, such teeth will first become mobile, then they will begin to fan-shaped and shift in different directions (under the forces of chewing pressure). In Fig. 11-13 you can see advanced forms of periodontitis in patients who, unfortunately, turned to the dentist too late. The teeth in these photographs have a very high degree of mobility and many of them only need to be removed.
Consequences of lack of treatment -
The most complete reminder for patients after tooth extraction
So, you left the doctor's office - the surgeon asked you to tightly squeeze a gauze pad with your teeth, which will help stop the bleeding. You need to hold it for about 20-30 minutes, that is, while you fill out the necessary documents at the clinic or go home. Remove the tampon carefully, moving it slightly to the side, without sudden movements, so as not to damage the fresh blood clot.
Very important! A thrombus (usually called a “blood clot”) protects the wound from microbes and prevents pieces of food and saliva from accumulating in the hole during the first week of rehabilitation. This is a natural sterile dressing that starts the process of new tissue formation. The most important rule that will protect you from complications and severe inflammation of the wound is to never remove the clot, do not touch it with your tongue or fingers, do not touch it with a toothbrush and protect it from other influences. Gradually it will resolve on its own.
Do not keep the tampon in place for more than 30 minutes - gauze soaked in blood and saliva will quickly become a breeding ground for infection. In addition, a blood clot is forming in the hole - the presence of a foreign body and additional injury are of no use to it. You need to give the wound the opportunity to heal naturally.
“If you have a complex tooth extraction, especially if you had surgery to remove wisdom teeth, or if you have an underlying condition, such as diabetes, you may need to observe a doctor for a few more hours.
For this purpose, we have our own hospital, where you can sit comfortably and relax while we monitor your condition to see if there are any complications. This will give us confidence that the operation will be successful and will reassure you as the patient.” Vasiliev Alexander Alexandrovich, implant surgeon, work experience of more than 9 years, make an appointment for tooth extraction WITHOUT complications!
The modern equipment of our clinic allows us to carry out the most accurate and comprehensive diagnostics. Consultation is free!
Sign up online
Swelling after tooth extraction (especially if it was complicated) can be prevented by applying a cold compress - to do this, wrap an ice pack from the freezer in a towel and apply it to the cheek (that is, from the outside) for no more than 20 minutes. After 15 minutes the procedure can be repeated. If you don't have ice on hand, frozen vegetables or meat will do, but be sure to wrap them in a bag and a towel to avoid cold burns. Cold constricts blood vessels, reduces pain and swelling, although it does not completely remove swelling. Compresses are effective immediately after surgery for approximately 3-4 hours.
Do not warm up the injury site under any circumstances! A hot compress will only make the swelling worse by increasing blood flow to the area of inflammation. This will lead to serious complications after surgery.
Incision healing time
How long will it take for the gums to heal after drainage is removed from it? On average, tissue regeneration takes 1-2 weeks. The process largely depends on the complexity of the previous operation and the individual characteristics of the patient. For example, in older people, wounds take longer to heal. This fact is explained by the slowdown of metabolic processes with age.
Complete gum regeneration may take more than 6 months. The wound healing process after opening the abscess takes place in several stages:
- the formation of a blood clot that protects the wound from the introduction of pathogenic microorganisms;
- formation of new granulation tissue (within 3-4 days from the moment of intervention);
- maturation of new epithelium (7-10 days from the moment of opening of the purulent focus);
- soft tissue regeneration;
- formation of young bone tissue.
After the operation, the dentist gives the patient a number of instructions that help maintain drainage in the gums and avoid the development of complications after the intervention. In the first 3-4 hours after the procedure, it is prohibited to consume food. During treatment, it is advisable to redistribute the chewing load to the healthy side of the jaw. Doctors also advise giving preference to dietary products.
In the postoperative period, it is necessary to avoid intense physical activity and avoid visiting saunas, swimming pools and baths. It is also important to give up bad habits - smoking and drinking alcohol.
Why is medical drainage used in dentistry?
Elimination of purulent diseases of the oral cavity often requires the installation of drainage. This product is a thin tube or strip. It can be rubber or latex. The material is moisture resistant, so it retains its qualities when in contact with saliva. Main functions of drainage:
- removal of purulent exudate from the source of inflammation;
- preventing wound healing until it is completely clean;
- providing access to the incision when it is necessary to introduce drugs into the infected tissue.
When the drainage is installed correctly, the patient almost does not feel it in the mouth. If you feel discomfort or even pain, you need to contact a specialist again.
Almost any disease of the oral cavity, during the development of which an infection is added, requires treatment with the installation of drainage. Most often these are dental diseases:
- pericoronitis – inflammation due to difficulty in teething (in adults this is an incorrectly positioned “figure eight”);
- alveolitis - the development of a pathological process in the socket after tooth extraction;
- periostitis - inflammation of the periosteum;
- periodontitis – involvement of the tissues that hold the tooth in the disease process;
- cyst or abscess, periodontitis
Suppuration may appear as a result of an injury (during complex tooth extraction, damage to the jaw, etc.). For the pathologies described above, drug treatment alone will not help. It is imperative to create an outflow of pus.
When is the procedure scheduled?
Drainage is necessary to remove purulent contents after a gum incision or tooth extraction. The passage of pus through a rubber tube is called the drainage process.
The procedure has 2 main goals:
- complete elimination of purulent exudate;
- preventing gum healing.
Saliva contains special substances that stimulate the regeneration of damaged soft tissues. Because of this, pathogenic microorganisms can remain inside the gums without having time to come out along with the necrotic masses. The condition provokes repeated exacerbation of inflammatory processes. In addition, epithelial cells are characterized by rapid division, which also contributes to the rapid healing of the wound after gum excision.
Drainage is required in cases where purulent formations in the oral cavity have been removed - abscess, gumboil, phlegmon. In this case, the doctor cuts the gum and places a drainage
For complete release of exudate from the wound, it is necessary to slow down the healing of the epithelium. A tape or tube type device does not allow the edges of the wound to converge prematurely.
How long does the drainage last? The answer to this question can be given by the surgeon after assessing the condition of the gums in the postoperative period. The device is removed after signs of swelling and inflammation of the soft tissue disappear.
If the tube is removed prematurely or not installed at all, the exudate will spread to nearby tissues and subcutaneous fat. The condition can cause dangerous infectious complications that lead to health problems, even death.
How long does drainage last after a gum incision? On average, this period is 1-2 days. The period can be extended after removal of abscesses and phlegmons to 1 week. If an infectious-inflammatory disease is accompanied by fever, then usually after installation of drainage this symptom disappears within a few days.
The installation is used not only after a gum incision, but also after tooth removal. Extraction in the first few days is also dangerous for the development of infectious complications. Installing a drainage tube reduces the risk of negative consequences and prevents gum infection.
The scheme is also used to accelerate the delivery of drugs to the pathological focus. This method simplifies the treatment of soft tissues located in hard-to-reach areas.
Flux is one of the common complications after tooth extraction performed with gum cutting
If the first signs of an abscess or flux occur, you should immediately consult a doctor. The methods of modern dentistry allow you to quickly and painlessly cope with the problem, while traditional medicine and self-medication can only aggravate the course of the disease.
When do you need dental help?
Flux has pronounced symptoms. The main one is the appearance of an abscess on the gum next to the diseased tooth. The abscess develops gradually. At first, the gums swell a little and a small red or whitish bump is noticeable on it. After some time, a noticeable fistulous tract forms on the lump, from which pus flows. The development of periostitis is accompanied by other symptoms:
- Swelling and swelling of the gums, lips, cheeks. Sometimes they can be so large that facial features are distorted.
- Severe cutting pain in the tooth area. Innervates the temporal region, orbits.
- The diseased tooth begins to become very loose, even if there was no mobility before or it was insignificant.
Since flux is caused by infection, it is characterized by symptoms that appear during any infectious process. The patient feels unwell, his temperature rises, his head hurts, and weakness appears. Lymph nodes on the head and neck become enlarged.
Any of these symptoms is a reason to consult a doctor. The more advanced the case, the higher the risk of complications. This disease is often accompanied by other pathological processes. For example, a cyst may form in tissues affected by infection.
Is it possible to cure an abscess at home?
Patients with acute conditions are admitted to dentistry without a queue. Therefore, if your health worsens, you should not postpone your visit.
The first question that a patient has is: why does pus appear in the gums and how to treat the pathology? The cause of infiltration is a weakened immune system and non-compliance with dental care measures. At the first symptoms of inflammation, you should immediately consult a dentist. Self-opening of a flux neoplasm threatens the addition of a secondary infection.
It is strictly forbidden to heat the inflamed area. Heat activates purulent-necrotic processes and accelerates the spread of infectious agents.
Timely sanitation of the inflammatory focus in a clinical setting prevents complications.
How long to keep gum drainage?
Since cases are different, the treatment required for different diagnoses is also different.
And only the attending physician can tell you exactly when to remove the drainage from the gums.
Removal of tooth drainage in most cases is done in a fairly short period - up to 3 days.
If the drainage needs to be changed, the dentist will definitely warn you about this and make an appointment for the day when the replacement will be carried out.
Sometimes you have to visit him every day, because the procedure for installing drainage on a tooth on your own at home is impossible.
During a routine removal of an inflamed wisdom tooth, for example, you can wear drainage for 1 day.
In other cases (for example, after a complex operation), you can walk with it for a week (as long as the course of drug treatment lasts).
A very important point: drainage should not greatly interfere with the person or cause pain.
In such cases, the drainage must be removed, the cut cleaned, and a structure made of a different material installed. Removing the drainage and inserting the one that has fallen out is best left to professional dentistry.
Gum recession: why gums recede
The formation of gum recession occurs when the surface of the tooth root is exposed. Without consulting a dentist, you will never be able to determine the exact reason why your gums are receding. This is due to a whole range of possible reasons, and in addition there are a large number of predisposing factors that make the risk of recessions more likely. Let's look at them.
1) Occlusal trauma, overload of teeth –
Occlusal trauma means that the contacts between your lower and upper teeth are not ideal, and in some areas there may be so-called “super contacts” (areas of premature overbiting). Normally, when the jaws are closed, the contact of the premolars, canines and molars should first occur, and only lastly the incisors. But if your incisors close first, then after all the other teeth have closed, they will experience overload, which will lead to bone resorption and a decrease in gum level (see photo below).
In addition to improper contact between the upper and lower teeth, bruxism (excessive uncontrolled clenching of the jaws, most often at night) can lead to occlusal injury. Patients usually refer to this condition as teeth grinding during sleep. You can learn more about this disease using the link above.
Exposure of tooth roots as a result of occlusal trauma:
Excessive chewing pressure on the teeth for a long time leads to resorption of the bone around them. Accordingly, in parallel with the decrease in bone level, there is also a decrease in the level of the gums, which primarily becomes noticeable in the area of the lower anterior teeth. For example, if you are missing part of your lateral chewing teeth, this leads to a redistribution of the chewing load on the remaining teeth, which will cause them to be overloaded. The front teeth are not physiologically designed for chewing at all - their function is to bite off food. In the absence of lateral chewing teeth, chewing food occurs with the front teeth, which quickly leads to their overload.
The absence of even 1 chewing tooth on each side can quickly lead to a decrease in the bite height in the lateral parts of the jaws, and this in turn will lead to excessive contact of the upper and lower front teeth (which will also cause bone resorption and gum recession with exposure of the roots of the teeth) . Moreover, a decrease in bite in the lateral parts of the jaws can occur not only due to the loss of several teeth. This can also occur due to excessive abrasion of dental tissues (on the chewing surfaces of molars), due to errors in prosthetics or restoration of teeth with filling materials, as well as as a result of the gradual abrasion of old fillings.
What to do - if you do not have missing teeth, then you need either a “gnathologist” or a very good orthopedic dentist to carry out “selective grinding of teeth” (this procedure will normalize the contacts between the upper and lower teeth, removing all “super contacts”) . If you have a reduced bite height in the chewing parts of the jaws due to the absence of some teeth, you need prosthetics. We are talking about replacing missing teeth with artificial crowns, replacing old fillings on the chewing surfaces of molars with ceramic inlays... But you need to start with a consultation with a prosthetist.
2) Chronic generalized periodontitis –
We have already said above that one of the main reasons why gums recede is their inflammation. It all starts with a completely harmless superficial inflammation of the gums (gingivitis), which is manifested by bleeding gums, their swelling and pain when brushing your teeth. But in the absence of treatment or improper treatment of gingivitis, the attachment of the gums to the neck of the teeth is gradually destroyed, inflammatory bone resorption and the formation of periodontal pockets begin to occur.
Reduced gum level due to gum inflammation –
When bone destruction reaches a certain degree, tooth mobility also joins the symptoms. Destruction of the periodontal attachment, bone resorption, periodontal pockets, tooth mobility - these are all symptoms of the next stage of gum inflammation, which is called periodontitis. Accordingly, because When periodontitis occurs, the level of bone tissue around the teeth decreases, and the level of the gums will also decrease.
Important: please note that a decrease in the level of gums in the area of 1-2 teeth is possible even with the most initial form of gum inflammation - even with catarrhal gingivitis. And for this it is enough simply to have microbial plaque in the area of the necks of the teeth (+ the presence of some predisposing factors, for example, a thin gum biotype). But with chronic generalized periodontitis, subsidence of the gum level occurs immediately in the area of a large group of teeth.
What to do - you need to start with a consultation with a periodontist (this is a dentist who specializes in the treatment of gum inflammation). Treatment of periodontitis includes not only anti-inflammatory therapy and removal of dental plaque, but also splinting of movable groups of teeth and prosthetic replacement of missing teeth. Therefore, in addition to consulting a periodontist, you may also need to consult an orthopedic dentist.
3) Incorrect movements of the toothbrush –
If you brush your teeth with a horizontal motion (instead of a sweeping motion) every day year after year, this can lead to gum recession - especially in the area of the lower front teeth. Typically, such patients not only have receding gums, but also hard tissue defects of non-carious origin appear in the area of the necks of the teeth. Incorrect brushing technique plays an important role in the formation of gum recession - especially in the presence of predisposing factors (thin gums, small height of attached gums, concomitant catarrhal gingivitis, etc.).
4) After correcting the bite with braces -
After correcting the bite with braces, you can often notice a decrease in the level of the gums. What I want to say here... There are only a few good orthodontists, so most of them plan orthodontic treatment without taking into account factors such as the height of the attached gum, the biotype of the gum, the thickness of the cortical plate of the jaw in the area of the teeth being moved. And as a result, we have what we have...
5) In the presence of predisposing factors –
Below we present a number of factors that sharply increase the risks of gum loss and root exposure. In some cases, they themselves can be the cause of gum recession (such as a highly attached frenulum of the lower lip), but most often they increase the damaging effects of the causes that we described above. These predisposing factors relate to the individual anatomical features of the gum structure in different patients.
- If you have a thin gum biotype, thin biotype means a small gum thickness. With the same force of the damaging factor, in patients with thin gums, recession will occur faster and be deeper than in patients with thick gums.
- Thickness of the cortical plate of the alveolus - if your cortical plate of the jaw (the front wall of the alveolus) is too thin.
Let's look at this using the example of the lower incisors. The anterior surfaces of the roots of the lower incisors are covered with a thin layer of bone, on top of which soft gum tissue is already located. In some patients, this layer of bone may be too thin (less than 0.5 mm), which, in the presence of a damaging factor, leads to too rapid bone loss, followed by a decrease in gum height. In some patients it can be even worse. For example, on the front surface of the roots of the lower incisors (in the area of their upper thirds) there may be no bone plate at all. In this case, the upper third of the roots will be covered only by the gum. This situation creates a risk of a recession, i.e. the fact that the gums will recede and the tooth root will be exposed - maximum.
- The height of attachment of the frenulum of the lips - for example, the frenulum of the lower lip may be attached too high to the gum edge, and then the movement of the lips (during conversation and facial expressions) will lead to the frenulum “tearing” the edge of the gum from the teeth. The same will apply to the low-attached frenulum of the upper lip.
- Insufficient level of attached gum – the gum is usually divided into “attached” and “unattached” (see photo below). Above the dotted line is the attached gum, and below it is the non-attached mobile gum. The peculiarity of the attached gum is that it is firmly fused with the underlying tissues and therefore immobile. The unattached gum is mobile, and its peculiarity is that it follows the movement of the lips and cheeks.
Very often the gum recedes on a tooth that has a very small height of attached gum. There is a clear relationship - the lower the level of attached gums, the higher the risk of recession (recession of the gums and exposed roots). When the level of attached gum is low, dentists often recommend performing special surgical operations on the gums, which can increase the level of attached gum and prevent exposure of the roots of the teeth.
Drug therapy
In the treatment of purulent processes, antibiotics are necessarily used. They reduce the risk of recurrent infection. Typically, your doctor will prescribe metronidazole with lincomycin or clindamycin. This combination of drugs allows you to act on gram-positive and anaerobic bacteria.
Metronidazole is prescribed orally, lincomycin and clindamycin are prescribed in the form of tablets or intramuscular injections. Lincomycin is used with caution, as this drug can cause allergies.
Metronidazole is prescribed orally, lincomycin and clindamycin are prescribed in the form of tablets or intramuscular injections. Lincomycin is used with caution, as this drug can cause allergies.
What to do if the drainage falls out?
What to do if the implant falls out of the gums prematurely? The answer to the question depends on the characteristics of the clinical case. If the swelling has subsided and the patient is not bothered by pain, then there is no need to contact the clinic to re-install the device. You cannot remove drainage from the oral cavity on your own even if the problem signs have completely disappeared.
Among the reasons for the installation to fall out on its own, the following should be noted:
- active rinsing of the mouth and thorough brushing of teeth;
- improper fixation of the structure over the tooth.
Re-installation is required if the gums still hurt after the rubber tube falls out. It is better if the procedure for installing the system is carried out by a doctor in a clinic. Only in rare cases do specialists allow patients to remove the drainage themselves when signs of swelling and inflammation disappear.
The procedure is carried out independently, taking into account the rules:
- Hands are washed thoroughly with soap.
- The oral cavity is treated with antiseptic solutions.
- The tape or tube is removed in front of a mirror. Grasp the free edge of the material with your thumb and index finger.
The procedure is accompanied by minor pain and blood loss. All of these signs are normal. You cannot interrupt treatment immediately after installing the tube.
The wound left after drainage should be regularly treated with antiseptics
How to rinse your mouth? Miramistin, Chlorhexidine solution, and hydrogen peroxide solution are suitable for this purpose. The procedure is necessary to prevent recurrence of the problem.
An abscess or gumboil is treated comprehensively. Pathology cannot be treated with medications alone. Therapy should include the installation of drainage, local treatment of the affected area and physiotherapeutic procedures carried out after opening the purulent focus.
What is drainage
Gum drainage has been performed by surgeons for many decades. It is a tube made of dense materials and its role in the treatment of infectious diseases can hardly be overestimated.
The invention was invented by a surgeon from France, Chassagnac. To create the structure, the doctor used glass and rubber. With the help of such a device, doctors could remove excess fluid and remaining necrotic masses from inflamed tissues. To achieve the desired effect, doctors left the tubes in the patient's body for several days.
And nowadays, surgeons use drainage during operations. However, the appearance of the devices has undergone significant changes: the tubes have become smaller and thinner in size, and modern materials are used to create them. The external drainage has changed, but all its functions have been preserved. It does not allow the incision in the gum to close prematurely; promotes the rapid removal of pus, ichor and necrotic masses from the affected areas; Helps drugs reach deep layers of soft tissue.
What drainage in soft tissues looks like in the photo
The drainage is left in the mouth until the swelling subsides. This sign indicates complete cleansing of the affected area. For speedy wound regeneration in the postoperative period, it will be necessary to use special ointments, gels and solutions for rinsing the mouth.
To create modern drainages, latex and rubber materials are used. Due to this, the patient practically does not feel discomfort when eating. Waterproof materials are firmly held in the gums and do not allow the tissues to tighten. A small section of the tube remains on the outside of the gum. Through it, pus is removed unnoticed by the patient.
How to place drainage in the gum
Conventionally, this procedure can be divided into five stages:
- Anesthesia of a specific area for manipulation or the entire jaw at once.
- The doctor makes an incision at the site of suppuration.
- Cleaning from pus.
- After this, the wound is disinfected.
- At the final stage, drainage is carried out.
Most often, drainage is installed once and does not need to be changed during treatment. An exception to this rule is a serious abscess or relapse of inflammation. In order for the tissues to grow together faster, if necessary, the dentist can use special dental adhesions or threads.
Tags
removal of a tooth.removal of a tooth.over a tooth.hood of a wisdom tooth toothache; wisdom tooth removal;brushing teeth and brushing teeth nearby with a soft toothbrush.tooth extraction or Dental prosthetics Prosthetics on Prosthetics on Prosthetics during Dental prosthetics Treatment Treatment process of treatment of diseases simplifies the treatment of soft ones; Interrupt treatment immediately; time of treatment is desirable Treatment of Methybefore timeliness of treatment and drug treatment. and treatment.
implantationpricesbite bracesarticleprostheticsservicesreviewsveneerschildrenwhiteningcrownsimplantshygiene