Posted by Marbery Gedrean | Checked by: Shteba Victoria Petrovna | Last revised: November 05, 2022.
What is a dead tooth? A healthy tooth has hard outer layers that allow the chewing organ to function normally. This is possible only thanks to the living tissue inside the tooth cavity and canals, which is called pulp. It plays a nourishing, sensory, protective and restorative role. A dead tooth, deprived of the benefits of living pulp, becomes brittle. It does not respond to painful stimuli and does not have regenerative properties. It is important to avoid dental necrosis by following the principles of oral health prevention. Let's look at what a dead tooth is and how it is treated
What is a dead tooth
A dead tooth is devoid of viable pulp, which disappears due to necrosis or root canal treatment. In the second case, the dentist removes infected formations from inside the chamber and canals.
Despite the pulp's enormous capacity for regeneration, when damaging stimuli exceed the limits of the tissue's protective properties, the cells eventually die. For this reason, pulp necrosis is classified as an irreversible pulpopathy. Necrosis may affect part or all of the pulp of a given tooth. In this regard, pulp necrosis is divided into partial and complete.
In the first case, a certain part of the cells dies, the remaining cells become inflamed, but remain viable. Partial pulp necrosis usually affects the tissues inside the tooth cavity and over time can spread into the root canals, forming complete pulp necrosis. A serious consequence of this condition is the spread of inflammation and infection to the periapical structures.
Delete or Treat?
There are two approaches to the treatment of periodontitis:
- Remove the problematic tooth and place a crown on an implant in its place. Such treatment, according to doctors, is faster and easier, and the result is more predictable.
- Doctors who recommend fighting for a tooth insist that your own tooth is always better, and it’s never too late to get an implant. They suggest using “every option” to save the tooth.
However, dentists do not always clearly explain that treating a “problem tooth” will require significant time and financial costs, but may not lead to the desired results. If efforts to save the tooth turn out to be in vain, then the cost of “prosthetics on an implant” will have to be added to the cost of “treatment”, since the absence of even one tooth in the jaw affects the position of neighboring teeth.
The choice of “treat” or “remove” is not very simple, since it depends on many factors. Let's figure out what guides a dentist when offering his treatment plan.
Tooth gangrene
The concept of a dead tooth is inextricably linked with the phenomenon of gangrene of the tooth, also classified as irreversible pulpopathy. When pulp cells die, they lose their protective abilities. The body also cannot independently cope with the removal of necrotic masses due to their location inside the hard structures of the tooth.
The conditions of the oral cavity provide putrefactive bacteria with an excellent environment for development. It is believed that if you leave everything as is without medical intervention, the dead pulp will sooner or later rot. This is dangerous because toxic substances produced by microorganisms damage healthy structures and lead to the spread of infection.
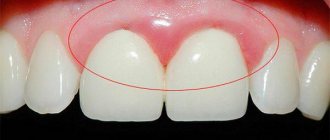
External difference
Doctors note that a tooth devoid of pulp can often be recognized by external signs. For example, immediately after living tissue has been removed from it, it may acquire a grayish tint, which will become darker over time. In addition, such a tooth stops reacting to cold and hot. One of the disadvantages is the fact that, even if such a tooth is damaged by caries, a person may not feel the destructive processes in a timely manner, since due to the lack of nerve endings he simply will not feel pain. Such a tooth, in addition, over time begins to gradually deteriorate and crumble.
Teeth guarantee. Why is it important to read a contract in dentistry? More details
How does a dead tooth form?
For a tooth to be considered dead, the pulp cells that have damaged or disrupted the tooth's supply of essential nutrients and oxygen must die.
Pulp necrosis most often occurs due to poor oral hygiene. Brushing your teeth at least twice a day, flossing, rinsing your mouth, and getting regular dental checkups can all protect you from developing tooth decay. If the rules of oral hygiene are not followed, cariogenic bacteria can colonize plaque deposits.
Microorganisms begin to produce numerous substances that demineralize the hard structures of the tooth, which leads to the formation of carious lesions. Thanks to breaks in the enamel and dentin, bacteria enter the chamber. In response to toxins produced by pathogenic microorganisms, the body reacts by developing inflammation.
Infection of the pulp significantly weakens its protective mechanisms, which leads to slow cell death. If necrotic masses become colonized by anaerobic bacteria, the process of decay begins and the infection can spread to neighboring structures.
Infection of the pulp resulting in a dead tooth can also occur as a result of a blood-borne infection. This occurs when an infected organ already exists in the body. Bacteria flowing with the blood settle in the pulp and cause a new source of infection. This scenario can occur with pneumonia, urinary tract inflammation, or tonsillitis, but infection of the hematopoietic pulp is rare.
Another cause of pulp necrosis is damage to the vascular nerve pedicle, which enters the tooth from the periapical region. The most common causes of this type of injury are mechanical factors that act with low intensity but over a long period of time. Situations in which the blood supply to the pulp may be compromised include:
- habit of biting nails, pens, pencils;
- setting teeth too quickly during orthodontic procedures;
- poorly fitting dentures.
In what cases is the nerve removed from a tooth?
First, let's look at why pulp removal (dental nerve) or depulpation is performed. The need for depulpation arises for several reasons. Practicing dentists identify the following indications for this operation:
- the occurrence of pulpitis: damage to the neurovascular bundle due to the spread of caries,
- extensive deep carious cavity: if the defect is more than 50% of the total volume of the crown, then a filling cannot be placed (it will not hold well and will quickly fall out), and other restoration options - pins, inlays, crowns - involve depulpation,
- the presence of several carious cavities: grinding down the enamel and removing infected dentin can significantly increase the size of the defect, i.e. again, the crown will have to be restored in such a way that pulp removal will have to be carried out,
- mechanical trauma: when a horizontal root crack is detected, for example, periodontitis: inflammation of the tissues of the ligamentous apparatus-1 surrounding the roots.
Symptoms of a dead tooth
The presence and severity of symptoms of a dead tooth depends on the degree of necrosis. If part of the pulp, including the nerve endings, remains alive, the patient will feel pain when eating hot food. To better determine the actual condition of the tissues inside the tooth, the dentist may use various tests. The viability test is carried out:
- Probing;
- use of ethyl chloride;
- pulpometer test;
- warmed gutta-percha.
These factors irritate the functioning sensory endings, which send pain impulses to the central nervous system.
In the case of total necrosis, the patient does not feel pain due to the destruction of receptors. He often pays attention to the darker color of the tooth and the dullness of the enamel. During a dental examination, the doctor notices the reasons that can lead to the formation of a dead tooth - carious cavities, extensive fillings, mechanical injuries.
The border between necrosis and gangrene is very smooth and often elusive, but is very important for the spread of inflammation and infection to adjacent tissues. To find out, the dentist will tap and palpate the periapical area. When the infection remains in the tooth cavity, the examination does not cause unpleasant discomfort from the surrounding tissues.
Inflammation at the root apex will become painful during the tests. Dental X-rays are also necessary for a more accurate diagnosis. They are an important guide in assessing the degree of inflammation and help plan further treatment.
In the case of gangrene, the patient reports bad breath and an unpleasant aftertaste. Typically a dead tooth does not cause pain.
Stuck root
The most common complication of tooth extraction can be a stuck, broken off root. If the root tip remains in the tissue, then the dentist has to use the entire arsenal of tools to get to the fragment: sometimes the tissue is drilled out or a section of the alveolus is removed to get to the desired depth. When hard tissues are crushed, this process can take quite a long time, since the dentist faces the difficult task of removing absolutely all the scattered fragments. In some cases this may take several hours.
Possible complications
The body is very difficult to deal with pulp infection due to the fact that it is covered by the hard structures of the tooth. Dead tissue in this area is almost always destroyed under favorable oral conditions. Although a dead tooth does not hurt, the infection spreads to nearby structures, causing a number of serious complications.
Inflammation and infection spread from the dead pulp to the periapical area, forming a periapical abscess. The disease goes through stages, forming a subperiosteal and submucosal abscess. Pain, facial swelling or redness, although distressing, are not the worst effects of these conditions. Bacteria around the mouth have easy access to various structures - not only the head, but also to distant organs. The spread of pathogenic microorganisms can cause brain abscesses, mediastinum, infective endocarditis or reactive arthritis.
Oral bacteria are also thought to be involved in triggering the development of autoimmune diseases in susceptible individuals. In extreme cases, microorganisms attacking the pulp can be a source of life-threatening sepsis, that is, the body's general response to infection with the occurrence of multiple organ failure. This is why so much emphasis should be placed on practicing good oral hygiene and responding promptly to diseased or dead teeth.
Generalized scheme for tooth extraction
The process of removing any tooth includes the following steps:
- Examination and collection of anamnesis (allergic status, information about the state of health and the dental apparatus).
- Preparation of the surgical field: treatment of the injection site, rinsing the mouth with an antiseptic.
- Anesthesia.
- Detachment of gum from tooth using a trowel.
- Loosening a tooth with forceps.
- Extracting a tooth from its socket.
- Treating the hole with an antiseptic.
- Stop bleeding with tamponade.
According to this scheme, simple removal is carried out. In some situations, for example, when a wisdom tooth or a badly damaged molar is pulled out, a complex extraction is required. Its main difference is that in addition to forceps, the dentist uses a drill to cut out bone tissue or saw the root into pieces, a chisel, a hammer and other dental instruments.
Wisdom tooth removal diagram
Getting rid of a wisdom tooth can be especially difficult. Due to its location in the posterior quadrant of the jaw, access to it is difficult. With anatomically incorrect or curved roots, which are often found in third molars, the dentist may be forced to make incisions in the gums, pull out the root piece by piece, and then apply sutures.
Whitening dead teeth
A beautiful smile is not only an aesthetic value, but also a guarantee of well-being and self-confidence. Even in such a case as a dead tooth, whitening is possible. Fortunately, root canal treatment does not prevent you from achieving your dream of a beautiful Hollywood smile.
Teeth whitening methods are divided into external and internal. The first type is used to lighten teeth with living pulp. The second option is recommended after root canal treatment.
Internal whitening methods are based on the introduction of bleaching agents into a chamber that are intended to lighten the tooth. The most popular bleach used by dentists is high concentration hydrogen peroxide (perhydrol).
Treatment is carried out after hygienization and protection of surrounding tissues from the toxic effects of the bleaching agent. After access through the crown, the doctor cleans the chamber, leaves bleach inside and temporarily closes the cavity. After a certain period of time (usually several days, depending on the material used), the patient returns to the chair and the dentist evaluates the effect. If necessary, the entire procedure can be repeated.
You can also find a thermocatalytic technique recommended in case of difficult to remove discolorations. This is a quick teeth whitening method. Thanks to the use of a special lamp that accelerates the action of the bleach, the patient can enjoy the effect immediately after the procedure.
Causes of darkening of pulpless teeth
The procedure is carried out solely at the request of the patient, as it mainly serves only an aesthetic function. Most often, forced lightening is required for dead incisors or fangs, since they are always visible, and if the shade of the enamel differs even by a couple of tones, it will be noticeable.
Teeth from which the pulp, that is, a collection of blood vessels and nerve endings, have been removed are considered dead. It is because of them that we feel pain, which warns of the presence of problems: the development of caries, internal trauma, etc.
In the absence of pulp, hard tissues cease to receive nutrition. What we see is no longer a tooth, but its shell, like a tree without roots. Such an incisor or molar will most likely not look the same, much less function. The consequences begin to be noticeable about a month after pulp removal. Dentin and enamel, as well as the main mineral part of the tooth, weaken and dry out. All these processes make the structure of solid tissue more porous.
Without constant replenishment, the tooth becomes defenseless and what was previously not a particular problem becomes more dangerous for it. It better absorbs pigments from food, for example, coffee, tea, alcohol, colored lemonades, berries and fruits, chocolate and other products with a high content of dyes. A pulpless tooth is like a sponge, so dyes accumulate in it faster, which means that after some time its shade begins to differ from the general tone of other teeth. If this is the reason for the color change, then standard whitening with an active gel is performed.
But there are also more complex problems when a canine or molar darkens from the inside. This happens precisely because of the removal of the pulp. Usually, those nerves that are damaged for one reason or another or interfere with the normal treatment of diseases such as tooth decay are removed. This removal may damage blood vessels, causing bleeding inside the canal. The dentin of a healthy tooth stains even more quickly than the enamel of dead hard tissue. Due to bleeding, the tooth becomes red and sometimes has a purple tint. In this case, standard bleaching will not help, since it mainly affects the outer layers of the fabric.
Treatment
Due to possible serious health consequences, it is imperative to treat a dead tooth. The dentist will first suggest root canal treatment. In situations where mechanical obstructions (calcification) or a certain root position prevent the endodontist from working, the alternative is hemisection (removal of one of the roots along with part of the crown), radiodissection (removal of one of the roots) or extraction (removal of the entire tooth).
Root canal treatment involves removing dead pulp from the chamber and canals of the tooth along with bacteria. After treating the carious lesions and accessing the inside of the tooth, the dentist removes dead matter from the inside of the crown and then begins to manipulate the root canals. To do this, he uses thin instruments and generously rinses the treatment area with antiseptic agents to kill all bacterial flora. The last stage of root canal treatment is closing the canals with a specialized material (usually gutta-percha) and restoring the crown of the tooth.
The pulp may not be completely dead, so the entire procedure is performed under local anesthesia. If its implementation turns out to be impossible (for example, as a result of an allergy to anesthetics or a coagulation disorder), root canal treatment is performed with devitalization (killing) of the pulp. During the first visit, the doctor injects substances into the tooth that cause tissue death. The destruction of nerve endings leads to the absence of pain, thanks to which the dentist can perform root canal treatment without anesthesia at the next session, and the patient does not experience any unpleasant ailments associated with the procedure.
Despite the fact that a dead tooth does not hurt after properly performed root canal treatment, it happens that the first days after the procedure can be marked by serious illnesses. They are caused by the reaction of surrounding tissues to actions in the operation area and pass quickly. If toothache occurs after some time, this may be a sign of developing infection and inflammation. Typically occurs as a result of:
- inaccurate removal of necrotic masses;
- survival of microorganisms, despite the use of special measures;
- leaky filling of channels;
- In this case, most often there is a need for repeated root canal treatment.
Causes of depulpation
There are a number of indications for dental nerve removal. Depulpation is most often carried out in the following cases:
- with extensive carious lesions affecting the dental nerve;
- development of infection in the dental canal;
- mechanical damage to the pulp;
- In the process of preparing for prosthetics, even a healthy pulp may be removed; this is necessary to eliminate the risk of developing re-inflammation in the tooth after the installation of an orthopedic structure.
The procedure for removing pulp from a tooth is performed in the following sequence: 1. Based on an x-ray taken, the doctor determines the structure and size of the dental canals. 2. Local anesthesia is administered. 3. The pulp is removed first in the coronal and then in the root part of the tooth. 4. Dental canals without pulp are carefully treated with an antiseptic solution. 6. After treatment, the canals are sealed. 7. Most often, a temporary filling is subsequently placed on the tooth, which later must be replaced with a permanent one.
Results
Dead tooth is the general name for a condition in which the inside of a tooth is filled with dead tissue or special materials after root canal treatment. If all pulp cells are necrotic, the patient does not feel pain. Due to the potential for serious complications, a dead tooth should be treated. Most often, root canal treatment is performed, and in case of contraindications, a fragment or the entire tooth is removed. The most common cause of a dead tooth is decaying bacteria, so good oral hygiene and regular dental checkups are the foundation of a healthy smile.
Cleaning canals under a microscope
Cleaning of the canals is carried out using modern microscopes, thanks to which the image is magnified twenty times or more. This allows you to carefully examine the internal condition of the diseased tooth. Even through a tiny hole equal to 1 mm, it is possible to conduct not only research, but also high-quality treatment, without complications and destructive effects on soft tissues.
Using microscopic equipment, the doctor:
- painlessly penetrates into the canals
- determine the number of branches
- preserves healthy tissue
A microscope can significantly facilitate the process and quality of canal cleaning. The dentist monitors his actions through a microscope during the procedure. Previously, X-rays were used for control, and with the use of microscopes, it became much more convenient to treat canals.
Features of whitening at home
Home whitening of a dead tooth is a very convenient method, but in this case it very rarely provides the required effectiveness. This is explained by the fact that at home, as a rule, products are used that only have an external effect. Sometimes such methods are not enough to lighten the enamel and without introducing special components into the tooth cavity it is simply impossible to return it to its natural shade.
At home, whitening gels are usually used, which, after penetrating the enamel, activate chemical reactions in it. It is necessary to work with such substances with extreme caution, since there is a high risk of not only damaging the enamel structure, but also damaging the mucous membranes. Therefore, it is best to trust such procedures to specialists who can prevent possible risks.