Retrograde filling is a method of filling root canals with access through the root apex. It is indicated if it is impossible to carry out this procedure using the standard algorithm. Most often, it is used if it is impossible to remove previously installed filling material from the canal, although there are a number of other cases when this method is indicated. With the right approach, it prevents the penetration of pathogenic microorganisms through the root canals into periodontal tissue and alveolar bone and ensures effective closure of the apex area (root apex).
The CELT Dentistry Department invites you to undergo retrograde canal filling in Moscow. We have all the necessary licenses and certificates and work on the basis of an official contract with a guarantee. Our dentists have decades of experience in scientific and practical work, in which they are supported by a powerful diagnostic and treatment base, as well as effective and safe materials of the latest generation. You can find out the price of retrograde filling by going to the “Services and Prices” tab. We regularly update our price list, but to avoid misunderstandings, we recommend that you check the numbers with our information line operators or at a doctor’s appointment.
Dentist consultation - 1,000 rubles.
Retrograde canal filling (RTA) - 9,000 rubles.
Removing stitches - 350 rub.
At CELT you can get advice from a dental specialist.
- The cost of a consultation with a dental surgeon is 1,000
Make an appointment
Indications and contraindications for retrograde filling
Indications
- Impossibility of re-treatment of canals due to incorrectly previously filled canals using cement, pastes or their analogues, which does not allow unsealing;
- Anatomical features of the structure of the patient’s root canals, which are too long or have a strong curvature, which do not allow full endodontic treatment or make it impossible;
- Obliteration of root canals of various natures, including inflammation, malignant neoplasms, age-related changes and medical errors;
- The presence of fragments of endodontic files, anchor pins or stump inlays in the canal, which did not allow it to be hermetically sealed;
- The presence of a restoration on the tooth in the form of a fixed prosthesis, made of porcelain or metal ceramics, along with one or more of the above contraindications.
Contraindications
There are specific contraindications, which include mobility of teeth of the third or fourth degree due to periodontitis. At this stage of the disease, bone resorption exceeds 50% of the length of the tooth root, and the depth of the periodontal pockets is more than five millimeters.
In addition, there are a number of general contraindications that do not allow surgical dental interventions to be performed in the oral cavity. These include:
- Pregnancy in women;
- Periods of menstruation;
- Blood diseases that are characterized by disorders of blood clotting;
- Diabetes mellitus in the stage of decompensation;
- Infectious diseases in acute form;
- Chronic pathological conditions during periods of exacerbation;
- The patient has neoplasms of a malignant nature;
- Mental disorders.
Materials used
The traditional retrograde filling material is amalgam. The advantages of amalgam include good shape retention and low shrinkage.
The use of amalgam is associated with a number of difficulties:
- the technology requires thorough drying of the cavity surface before filling with material;
- excess amalgam getting on the tissue leads to darkening of the gums, which is undesirable in the smile area;
- The technique is quite labor-intensive.
Regular development of innovative dental materials for filling allows manipulations to be performed with less time and good quality.
COE
Zinc oxide eugenol cements (ZOE) are made from eugenol and zinc oxide mixed in certain proportions. This composition hardens in 10-12 hours.
The positive properties of COE include the following characteristics:
- inertness to dental tissues, have good biological compatibility;
- work as additional antiseptics;
- thermal conductivity is low,
- do not affect the change in color of hard tooth tissues.
In terms of their manipulation and physico-chemical properties, COEs are inferior to varieties of other dental cements.
This type of cement is used for the following purposes:
- installation of temporary fillings;
- performing manipulations for intermediate dental restoration;
- fixation of therapeutic inserts required in the treatment of deep carious cavities;
- installation of crowns, both permanent and temporary;
- securing gaskets to provide thermal insulation;
- sealing the root canals of the anterior teeth;
- fixation of gingival dressings with medications.
The most popular COEs are represented by the following names: “Cariosan” (DentalSpofa), “Cavitec” (Kerr).
COEs containing eugenol inhibit the polymerization reaction, so combined use with composite materials is undesirable.
Intermediate restoration pastes
This material makes it possible to perform manipulations in periapical tissues. The results of using these pastes make it possible to fill a dental cavity more reliably in comparison with the traditional material - amalgam.
The material used in modern dentistry for filling root canals, the procedure technique.
In this publication we offer reviews from experts about cement fillings on teeth.
Follow the link https://www.vash-dentist.ru/lechenie/zubyi/kofferdam-v-stomatologii.html to become more familiar with the types of rubber dam used in dentistry.
Super-EBA
An improved version of COE is Super EBA cement. The components of the material are:
- liquid fraction : a) eugenol – 37.5%; b) ethoxybenzene acid – 62.5%;
- powdery fraction : a) zinc oxide – 60%; b) aluminum oxide – 30%; c) natural polymer – more than 6%.
The practical use of Super EVA cement gives good results (more than 96% of patients experienced healing after a year).
Super EVA cement occupies an intermediate position in quality between COE and glass ionomer materials.
The preparation of a working cement mixture is done as follows:
- A small amount of the liquid fraction is applied to the surface of the glass and generously sprinkled with a powdery composition. The result of mixing should be a homogeneous shiny mass with good adhesion to the glass surface.
- The resulting mass is carefully rolled into a cone approximately 1 mm thick and up to 3 mm long.
- Filling is performed in portions. To speed up the hardening of the cement mass, it is recommended to cover the finished filling with a hot, damp cotton swab.
- Excess cement is removed with a round plugger, a curette, then everything is polished with a diamond-tipped bur.
Intermediate and final results of the work are examined under microscopic magnification.
Glass ionomer cements
Modern filling materials are represented by glass ionomer cements, which receive excellent reviews from dentists.
Glass ionomer cements (GIC) have a heterogeneous structure, which is filled with aluminosilicate glass . Polyacrylic acid serves as a framework for the matrix.
In practice, GICs are used as materials for restoring and filling teeth, and also as insulating liners.
In addition, polyacrylic cement may contain polyitaconic, polymylenic acid. The following components can be used as a catalyst:
- hydroxyethyl methacrylate;
- wine acid;
- camphorquinone.
The powder fraction is composed of the following substances:
- the addition of quartz gives greater transparency , lengthens the setting time (the dentist has a reserve of time when working), and the strength characteristics of the cement are somewhat reduced;
- aluminum oxide reduces working time , gives greater strength, acid resistance and opacity;
- calcium fluoride increases strength , imparts color rendition and resistance to the effects of carious processes;
- Aluminum phosphates make it possible to select color shades , stabilize the structure, and increase strength;
- barium salts and inclusions of other metals allow radiography to be performed with greater contrast.
The advantages of glass ionomer cements are the following:
- practicality of use, the composition fills prepared cavities in 1-2 stages of application, while dentin and enamel do not require an etching procedure;
- performance of the material in humid environments;
- provides excellent adhesion along the edges of the wall being filled;
- excellent adhesive properties with metals, clove oil;
- the ability to release fluoride ions to dental tissues after filling throughout the year;
- has low shrinkage values;
- inertness towards dental tissues;
- thermal expansion matches the natural values of natural teeth.
It is impossible not to mention the presence of such disadvantages of the GIC:
- the cement mass hardens to normal limits within a day;
- the material is hygroscopic during the first day; ions may be washed out or released insufficiently;
- It is not advisable to treat fresh fillings with burs; vibration destroys the integrity of the composition;
- low wear resistance of fillings;
- low aesthetic component;
Among GIC, the most popular is Vitremer, VOCO, which has a triple degree of curing, while being easy to use and aesthetically pleasing.
The essence of retrograde root canal filling and the materials used
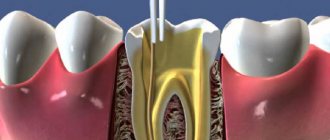
The essence of retrograde root filling is apicoectomy or resection of the root apex. This is a surgical operation that is aimed at removing the apical part of the tooth (including the pathological focus, if any). Having gained access to the canal, the dental surgeon processes and seals it.
Amalgam for retrograde tooth root filling
Despite a number of significant advantages, this material is used less and less often, since it can cause darkening of the gums, and the filling method is too labor-intensive. Today it is being replaced by modern materials that significantly simplify this procedure. At the same time, it is worth noting a number of advantages of amalgam:
- Ability to maintain a given shape well;
- Minimal shrinkage.
Zinc oxide eugenol cements for retrograde tooth root filling
COE are materials based on eugenol and zinc oxide. They are well compatible with dental tissues, as well as:
- Absolutely inert to them;
- They have antiseptic properties;
- Do not cause changes in hard dental tissues.
Their hardening time ranges from ten to twelve hours.
Glass ionomer cements for retrograde filling of tooth canals
GIC is the latest generation of materials with excellent strength and aesthetic properties. They are not susceptible to carious processes, allow you to select the desired shade, and provide radiographic contrast. Their other advantages:
- Functionality in wet environments;
- Excellent adhesion to different materials;
- Release of fluoride ions during the first year;
- Minimal shrinkage.
Materials
The standard retrograde filling procedure is performed using amalgam. Its main advantages are:
- minimal shrinkage;
- ability to hold shape.
It is worth noting that the use of this material is accompanied by some difficulties:
- the need for thorough drying of the surface of the cavity to be filled;
- impossibility of use in the smile area, which is associated with the likelihood of darkening of the mucous membrane;
- labor intensity.
Leading dental clinics regularly develop innovative filling materials that make it possible to reduce the labor intensity of procedures and at the same time improve their quality.
These include:
- zinc oxide eugenol cements (ZOE). The most popular lines: Cariosan, Cavitec, Dental Spofa, Super-EBA;
- pastes for intermediate restoration;
- glass ionomer cement compositions (GIC). The VOCO and Vitremer lines are considered the most popular.
Stages of manipulation
The procedure is carried out according to the following scheme:
- Administration of local anesthesia. As a rule, submucosal infiltration is performed, but in some cases it is necessary to use transcortical anesthesia of bone tissue.
- Separation of the gingival area from the jaw bone. To do this, the doctor makes incisions.
- Resection of the root apex (before identifying the dental canals).
- Treatment of the cavity with anti-inflammatory and antiseptic drugs. In the presence of extensive purulent foci, this manipulation is carried out several times.
- Hermetically filling the prepared cavity with filling compounds followed by polymerization.
- Repeated treatment with antiseptics.
- Cutting off excess filling material.
- Bringing the detached area of soft tissue to its original state by applying sutures.
Sutures are removed on the fifth to eighth day after the intervention. After the procedure, patients are prescribed a three-day course of radiotherapy.
After surgery, the doctor re-orders an x-ray to correct any inaccuracies (if any are identified).
Reviews of doctors providing the service - Retrograde root canal filling
I would like to express my gratitude to the dentist Elena Nikolaevna Kiseleva and her assistant Svetlana - they are real specialists and at the same time sensitive, not burnt out by years of practice.
Thanks to them, I have been coming back here for many years. Thanks to the management for such doctors! Read full review Svetlana Nikolaevna
13.08.2021
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights. Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review
Sofia
28.12.2020
Modern requirements for conservative-surgical methods of tooth preservation
Yu. G. Trofimova assistant of the department of propaedeutics of dental diseases of St. Petersburg State Medical University named after. ak. I. P. Pavlova
I. G. Trofimov Ph.D., Associate Professor of the Department of Surgical Dentistry, Faculty of Medicine, St. Petersburg State University
G. A. Khatskevich Doctor of Medicine, Professor, Honored Doctor of the Russian Federation, Head of the Department of Pediatric Dentistry with a course of Maxillofacial Surgery at St. Petersburg State Medical University named after. ak. I. P. Pavlova
Foci of chronic odontogenic infection often cause tooth extraction, despite the effectiveness of conservative and surgical treatment methods. When asking the question “should I save a tooth or not?”, it is necessary to understand what tooth-saving techniques can be used in each specific case and what results the specialist and the patient can expect. Predictability of results in medicine is a complex issue, however, relying on experience, skill, good tools and materials, and support from the patient, this issue can be resolved positively for both parties.
Among specialists in the field of endodontics, it is customary to begin the elimination of foci of chronic odontogenic infection with conservative treatment. Accurate implementation of the protocol for mechanical and medicinal treatment of the root canal system with subsequent high-quality obturation allows us to achieve a reduction in pathological periapical changes in most cases.
According to various studies, the success rate of conservative therapy during primary endodontic treatment varies from 53 to 98% (Saunders WP, 1994, Kerekes K., 1979, Jokinen MA, 1978). With repeated endodontic treatment (refilling of root canals), the success rate of conservative treatment of foci of chronic odontogenic infection is reduced to 60-74% (Bergenholtz G., 1979, Gorni FG, 2004, Trope M., 2005).
The morphological characteristics of the odontogenic lesion influence the choice of treatment tactics. It is a generally accepted fact that chronic granulating and granulomatous periodontitis can be cured quite well after conservative therapy. However, the issue of conservative treatment of cysts is controversial (Nair PN, 1998, Nair PN, 2003). According to experts in the field of endodontology, conservative treatment of a cyst that is odontogenic in nature and size within 5 mm can lead to its complete reduction.
Surgeons believe that to achieve complete reduction of a cyst-type lesion, its surgical removal is necessary. From the point of view of the etiopathogenesis of the process, it can be assumed that reduction of an odontogenic cyst as a result of conservative treatment is possible, which is confirmed by clinical experience.
A true cyst must definitely be removed surgically [5].
When does the need arise for surgical treatment of foci of chronic odontogenic infection?
Numerous studies have shown that only 10% of periapical lesions require surgical intervention as an adjunct to successful root canal obturation [5]. However, during primary and especially repeated endodontic treatment, a number of complications may arise, such as breakage of endodontic instruments in the root canal, root perforation, canal transportation, and the formation of microcracks.
Numerous studies have shown that only 10% of periapical lesions require surgical intervention as an adjunct to successful root canal obturation
Thus, in some clinical situations, a surgical approach may be more effective than repeated endodontic treatment. Especially when we encounter odontogenic lesions in the area of teeth where restorations using pins or orthopedic structures have recently been performed. Removal of a crown, post or root inlay, or repeated endodontic treatment can lead to complications, take longer, cost more and be less predictable than the results of surgery.
Previously, when the operation of resection of the root apex, especially the lateral teeth, was rare, this type of treatment was the last attempt to save the tooth.
Today, surgical endodontics is an alternative or addition to the conservative treatment of foci of chronic odontogenic infection (in case of unsatisfactory results). Also, the surgical method of treating foci of chronic odontogenic infection should be preferred in the presence of extraradicular infection and large cysts. It is generally accepted that in patients with a reduced immune status and the presence of aggravating somatic pathology, foci of chronic odontogenic infection are much less susceptible to regression, and surgical sanitation is recommended for such patients.
Changes over the past decade have improved surgical techniques, increasing the success rate to 92% (Von Arx, 2003, Taschieri, 2006, Kim, 2008, Saunders, 2008) compared to the traditional approach - 61% (Frank, 1992, Friedman, 1993, Kvist, 1999, Rahbaran, 2001).
The impetus for the development of new instruments, materials and modifications of the technique was a deeper understanding of the possible paths of infection in the complex root canal system, a detailed study of the anatomy of the apical part of the root and an analysis of the problems that arose when using the traditional method of surgical treatment. The use of microinstruments and ultrasonic tips for retrograde preparation , biologically compatible materials for retrograde filling and magnification technology during surgery are the main components that determine the modern surgical approach to the elimination of periradicular pathology, allowing to achieve a high probability of reduction of the pathological focus and a predictable result even with long-term observation.
However, the development of new tools and materials requires adherence to certain technical rules at various stages of the operation. Especially at the stages of formation of the “apical control” zone. The concept of the “apical control” zone implies a 3 mm resection of the root apex without creating a bevel, retrograde preparation with ultrasonic instruments to a depth of 3 mm along the tooth axis and hermetically sealed retrograde cavity filling with biocompatible materials. It is during this stage that we encounter the main differences between the traditional and modern approaches when performing apicotomy surgery.
The traditional apicotomy technique involved creating a bevel at an angle of 45-60 degrees. The need for this stage was determined by improved conditions for visualization, easier access to the root canal and the use of large instruments (Rud J., 1972, Gutmann JL, 1985, Gutmann JL, 1991, Gutmann JL, 1993).
According to Kim S., 2001, Kim S., 1997, creating a bevel leads to tissue trauma: excessive removal of the cortical plate, an increase in the volume of osteotomy, greater opening of the dentinal tubules, the danger of lingual perforation and the creation of an endo-periodontal communication.
For a long time there was no consensus on how much of the root should be resected to satisfy biological principles? Initially, root resection was carried out to the level of filling material in the root canal or to the boundaries of the pathological focus, which led to unnecessary tissue removal and worsening tooth retention. In 1994, Gilheany et al. recommended resecting 2 mm of the root apex to minimize bacterial contamination from the canal. In their study, Kim S. et al. (1991) determined that with a resection volume of 3 mm of the root apex, 98% of the apical ramification and 93% of the lateral canals were removed.
Since a 4 mm resection will produce similar results, a 3 mm resection is more recommended, whereas a 2 mm resection does not eliminate as much lateral canal and apical arborization, which may lead to reinfection and subsequent failure. After resection of the apex, it is necessary to examine the resected root surface. In the absence of adequate canal tightness created with the help of root filling material, the need arises for its retrograde filling.
For a long time there was no consensus on how much of the root should be resected to satisfy biological principles? Initially, root resection was carried out to the level of filling material in the root canal or to the boundaries of the pathological focus, which led to unnecessary tissue removal and worsening tooth retention
To carry out this stage with special care, it is necessary to have good lighting, the use of magnifying equipment, micromirrors and identification of anatomical structures, and staining of the resected surface with a solution of methylene blue.
During the surgical procedure, two main questions must be resolved: is it sufficient to perform only resection of the root apex in cases of adequate obturation of the root canal system, or is it necessary to carry out retrograde preparation in each case?
If the root canal is obturated well and the root filling in the area of the apical cut is adequate, dense, with good marginal fit, there is no need for retrograde filling. However, if the root filling is not airtight, there is a need for additional retrograde preparation and root filling [11].
Inadequate sealing of the root apex is the main cause of periapical damage and the source of the release of microorganisms and their toxins outside the root. Accordingly, removal of pathologically changed tissues in the area of the root apex only through periapical curettage will subsequently lead to a relapse, since it eliminates only the effect, and not the main cause. At the initial stage, clinical improvement and even radiological improvement is observed, but this phenomenon is temporary.
Thus, there is agreement among endodontists that inadequate filling, untreated accessory canals or the isthmus zone provoke the occurrence of periapical pathology. Surgical treatment involves not only removal of pathological tissue and resection of the root apex, but also retrograde obturation of the root canal system.
In a study by Altonen & Mattila (1976), tissue repair and treatment success were observed more frequently in the retrograde sealing group compared with the nonretrograde sealing group.
Lustman (1991) and Rahbaran (2001) observed improved tissue recovery after surgery in cases where retrograde root filling was performed with amalgam or SuperEBA, compared with groups where retrograde preparation was not performed. Some studies have shown no significant difference between groups (Rapp, 1991, August, 1996).
In the results of the Toronto Study (2004), after repeated endodontic treatment followed by resection of the root apex, complete recovery was observed in 7 out of 8 cases. Thus, careful mechanical and medicinal treatment of root canals and their obturation followed by resection can provide a high percentage of recovery. However, in the molar area, the anatomy of the root canal system is more complex and difficulties can arise.
From the experience of many clinicians, there is an opinion that the positive result in cases of retrograde filling is longer than without it. It is easier to achieve a long-term positive result after surgical intervention in frontal teeth than in multi-rooted teeth. This is due to technical difficulties in performing the operation and features of the anatomical structure.
An important anatomical structure that has received attention in recent years is the isthmus zone in root canals. The isthmus is a narrow part that connects the main large anatomical structures.
Until 1983, the isthmus zone was not even mentioned in the dental literature in relation to the apicotomy operation. In 1983, an article first appeared in a Canadian dental journal describing the isthmus zone, Camburizzi & Marshall (Molar endodontic surgery). Before 1990, information about the need for debridement and retrograde filling of the isthmus area was virtually absent from the literature. But the isthmus area is part of the root canal system, not a separate structure, so it must be cleaned, shaped and filled in the same way as other canal spaces.
An important anatomical structure that has received attention in recent years is the isthmus zone in root canals. The isthmus is a narrow part that connects the main large anatomical structures.
Most often, an isthmus occurs between two canals located in the same root. As a rule, this is a group of molars and premolars. At the level of the apical 3 mm, the isthmus is detected in 90% of the medial buccal root of the upper first molar, 30% of the upper and lower premolar, more than 80% in the medial root of the lower first molar (Kim S., 2001, Hsu, 1997). Such a high percentage of the occurrence of the isthmus zone indicates the need for attention to this zone when performing apical surgery.
This is another reason why in the molar area, apex resection without retrograde filling may fail. The root apex usually has a round shape, but after resection of 3 mm of the root apex, the canal space has an oblong shape and staining the cut area with methylene blue makes it possible to identify the isthmus zone [5].
According to the observations of foreign authors, a common reason for the unsuccessful result of surgical intervention in the area of the root apex of molars is the lack of treatment of the isthmus, since preparation with burs and filling with amalgam does not allow these stages to be carried out delicately.
The main purpose of retrograde preparation is to remove filling material from part of the canal, creating a cavity that can be adequately filled. Ideally, a retrograde cavity is defined as class I, 3 mm deep, with parallel walls along the axis of the canal (Garr GB, 1997).
When preparing a root section using burs with a micro-head tip, the following problems arose: difficult access, risk of root perforation, insufficient depth of treatment, opening of dentinal tubules after resection of the root apex due to the creation of a bevel, inability to remove necrotic tissue from the isthmus area. The advent of ultrasonic tips for retrograde preparation has greatly facilitated this stage, allowing you to quickly and gracefully form a retrograde cavity, bypassing the difficulties that arose when working with burs.
In 1957, Richman first introduced the use of ultrasound in endodontics, using a modified ultrasonic periodontal scaler to remove plaque during apicotomy. In 1992, Garr GB introduced specially designed retro-attacks for retrograde preparation. In 1995, Engel et al. published their observations on the use of ultrasonic tips and their comparison with bur preparation, emphasizing the possibility of more convenient operation of the tips along the axis of the canal and a reduction in the risk of perforation.
A similar comparative characteristic was presented in their study in 1994 by Wuchenich et al., noting that when retrograde preparation is carried out with ultrasonic tips, the cavity is disinfected by removing infected dentin, and the cavity is formed deeper, which contributes to better retention of the filling material.
Advantages of working with ultrasonic nozzles:
- Convenient surgical access.
- There is no need to create a bevel.
- Formation of a cavity along the long axis of the root.
- Creation of sufficient preparation depth.
- Cleaning the root section and isthmus area from dentine filings.
- Relative smear layer removal.
Despite these advantages, in 1994 Saunders et al. in an experiment on extracted teeth, the formation of microcracks was discovered due to retrograde preparation with ultrasonic tips, Berutti file (EMS), which, according to the authors, could lead to increased microleakage in the area of the apical section of the root.
However, in 1996, Layton et al. suggested that this study was conducted incorrectly because the experiment was carried out on extracted, demineralized and dehydrated teeth and in the absence of surrounding periradicular tissue, and in this condition the tooth structure is predisposed to the formation of cracks. In 1995, Walpington et al. recommended that when performing retrograde preparation with ultrasonic tips, follow the operating mode for two minutes at low or medium power to minimize the risk of crack formation.
Studies conducted on cadavers (Calzonetti KJ et al., 1998, Gray et al., 2000) have shown that preparation with ultrasonic tips does not cause crack formation. In a study by Morgan LA et al. (1999), carried out on 25 patients who underwent surgery, after which an impression was taken with a polyvinylsiloxane mass, only a slight formation of microcracks was found in the area of \u200b\u200bone root.
Developments in the design of attachments and materials for their manufacture continue with the goal of creating attachments with effective cutting ability with minimal risk of microcracks during their use. But it is clear that the use of ultrasonic tips in endodontic microsurgery has made this procedure more effective and simpler.
A retrograde cavity prepared by ultrasound according to class 1 must be filled with a material capable of providing a hermetically sealed filling of the resected root apex. In 1996, Torabinejad and Pitt Ford conducted an extensive review of retrograde filling materials. Previously, amalgam was often used for this purpose, but in the last decade, materials based on zinc oxide eugenol (IRM and SuperEBA) have been preferred.
Many studies have proven the high degree of tightness and biocompatibility of zinc oxide eugenol materials compared to amalgam (Szeremeta - Brower, 1985, Bondra DL, 1989, Pitt Ford TR, 1994, Pitt Ford TR, 1995). And the mineral trioxide aggregate (MTA), which appeared relatively recently, is recommended as an ideal material for retrograde filling. The exact composition of MTA is the property of the manufacturer, but the main ingredients are tricalcium silicate (Ca3Si), tricalcium aluminate (Ca3Al), tricalcium oxide (Ca3O2).
A retrograde cavity prepared by ultrasound according to class 1 must be filled with a material capable of providing a hermetically sealed filling of the resected root apex
The material is becoming increasingly popular due to its high tightness and biocompatibility. In in vivo studies, MTA has demonstrated the ability to induce the formation of bone tissue, dentin and cementum (Torabinejad M., 1997, Thomson TS, 2003, Baek SH, 2005). Compared with amalgam and SuperEBA used for retrograde fillings, MTA promotes the regeneration of periapical tissues, including the periodontal ligament and cementum.
For the same reasons, MTA is used for direct pulp capping and canal therapy. The results of assessing the inductive capabilities of MTA on bone tissue and dentin (Shin S., 2004) showed that cell cultures of osteoblasts and dentinoblasts of animals and humans grow faster and better in the presence of gray MTA than in its absence. The results obtained from animal experiments and in vitro laboratory methods provide unequivocal evidence that MTA has a high healing potential and is the most biocompatible retrograde filling material known to date, ideally suited for this purpose.
Experimental clinical results confirm the results of scientific research (Torabinejad M., 1997). But using MTA alone does not guarantee a successful result. When working with MTA, it is necessary to take into account the peculiarities of the technique of its use and the use of special tools. Clinical studies evaluating healing using MTA and IRM in microsurgical techniques following the use of ultrasonic preparation did not show significant differences in results (Chong BS, 2003).
Strict adherence to the surgical protocol is more important than the material used for the retrograde filling. Thus, the issue of using amalgam as a material for retrograde filling has been controversial since the development of modern microsurgical techniques and the use of materials with an inductive effect on tissue (Chong BS, 2003) [11].
All of the above evidence leaves no doubt that a correctly performed technique of endodontic treatment and surgical removal of foci of chronic odontogenic infection will provide a positive long-term result, which is what we observed in our study.
Materials
In the period from 2005 to 2010, at the State Medical Clinical Hospital No. 2 (St. Petersburg), we treated 152 patients with foci of chronic odontogenic infection (odontogenic cyst, chronic granulating and chronic granulomatous periodontitis). In 59.9% (91 people) of patients, conservative treatment was performed, achieving complete reduction of the pathological focus. Conservative surgical treatment was performed in 40.1% (61 people) of patients. In this group of patients treated with conservative surgical techniques, 27.9% (17 people) required additional retrograde filling.
Retrograde preparation followed by retrograde filling was performed in 27.9% (17 people) of patients from the group treated with a conservative surgical method on 30 teeth (25 frontal teeth (83.3%), 4 premolars (13.3%), 1 molar (3.4%). Diagnoses: odontogenic cyst - 14 patients (82.3%), chronic granulomatous periodontitis - 3 patients (17.7%). Of 17 patients, 6 people (35.2%) were diagnosed with relapse after previous resection of the root apex (patients from other medical institutions).
Methods
Examination. Patients underwent clinical examination using standard methods. The size of the pathological focus, the condition of periodontal tissues, the presence of tooth mobility, the condition of restorations, the condition of occlusion, and previous treatment were taken into account. Before surgery and to assess the result 12 months after surgery, patients were diagnosed using dental volumetric computed tomography. We consider this type of diagnosis to be reliable and invaluable at the stages of treatment planning and monitoring the effectiveness of the intervention.
Surgical intervention was performed using the following technique.
Anesthesia
Local anesthesia in the form of submucosal infiltration was carried out with articaine-based anesthetics Septonest 1:100,000 (Septodont), Ultracain DS (Hoechst GmbH). In case of a deep location of the pathological periapical lesion and dense bone tissue, additionally after detachment of the flap, transcortical anesthesia was performed using a QuickSleeper computer syringe (DHT) and a rotating Transcort-S needle (DHT). Additional injection of anesthetic directly into the bone tissue ensured almost complete painlessness during surgery and patient comfort.
Flap selection and access creation
Depending on the clinical situation, we used the following types of flaps: mucoperiosteal flap with a monolithic gingival edge, mucoperiosteal flap with preservation of gingival papillae (Velvart), submarginal rectangular Luebke-Ochsenbein flap.
The incision was made with a No. 15 blade. To detach the flap, a raspator, a Kirkland knife, an Orban knife, and a set of instruments for periosurgery Hu-Friedy were used. A combination of a fissure and cylindrical bur, and a ball-shaped cutter was used to perform an osteotomy and create access to the pathological focus.
Typically, 3 mm of the root apex was resected at an angle of 0–10 degrees using a Lidemann fissure bur under sufficient water cooling. Periradicular curettage was performed with a Lucas curette and periodontal curettes.
The resected root surface was stained with methylene blue and inspected using micromirrors (ObturaSpartan). When examining the resected root surface, attention was paid to the tightness of the root filling, the presence of cracks, perforations, the presence of additional canals, apical branches, and the unsealed isthmus area between the canals. If necessary, magnification was used using a magnifying glass or endoscopic equipment Karl-Storz-Endoskope (Germany) and a Cold Light Fountain 485 illuminator.
As an additional antiseptic treatment, the root section was coagulated using an Elektrotom R 200 coagulator (Berchtold Modul System GmbH). This technique was proposed by prof. Khatskevich G. A.
Carrying out retrograde preparation of a root section
In our practice, when performing retrograde preparation, we use ultrasonic attachments from EMS - Berutti, RE2 files. Berutti files are diamond-coated instruments for retrograde root canal preparation. The conical shape of the instrument allows you to quickly and delicately prepare a retrograde cavity. Files are used with 120 and 180 degree endochucks.
RE2 files are tools for processing the isthmus of the root canal. The surface of the nozzle is coated with titanium nitride to improve abrasive properties, used with 120 and 180 degree endochucks. These attachments allow you to quickly and effectively form a retrograde cavity of the required depth. When working with these attachments, you need to use the “endo” mode with water cooling with saline solution or sterile purified water. The operating time of the nozzle is usually 2-3 minutes.
Implementation of hemostasis
Hemostasis in the wound was carried out using a collagen hemostatic sponge.
For additional hemostasis, ferrous sulfate preparations Viscostat & Astrigedent (Ultradent Products, Inc., UT) were used. After ferrous sulfate was applied and hemostasis was achieved, the drug was carefully removed with saline to avoid affecting subsequent healing processes.
Transcortical anesthesia with anesthetics with vasoconstrictors provides an additional hemostatic effect, which is an important factor when performing periradicular surgery.
Filling a retrograde cavity
The retrograde cavity was treated with 2% chlorhexidine, sterile water solution and conditioned with 17% EDTA. The retrograde cavity was then dried with sterile paper points and obturated with ProRoot MTA (Dentsply). The material was introduced using a special carrier Dovgany tool and packed. A sterile napkin was placed in the bone cavity to prevent MTA particles from entering the wound.
Filling the bone defect and fixing the flap
If necessary, the bone defect was filled with bone chips and platelet clot or (optional) synthetic materials based on betatricalcium phosphate Syntho Graft 500-1000 um (Bicon USA), xenogeneic bone material Bio-Oss S 0.25-1 mm and L 1-2 mm (Geistlish), resorbable two-layer membrane Bio-Gide perio (Geistlish). The flap was then placed in place and secured with Ethilon 5/0 suture material (Ethicon USA).
results
In 95% of cases, we observed a successful result of conservative surgical treatment. Relapse phenomena were observed in 5% of patients after 5 years in the molar group.
In the group of patients where resection of the root apex was accompanied by retrograde filling, no relapse was observed. When X-ray analysis of the results obtained after 12 months on DOCT sections, we observed a complete reduction of the pathological focus, restoration of the bone tissue structure, the formation of a periodontal gap in the area of the resected apex and retrograde filling with MTA material, and the tightness of the retrograde filling. The absence of clinical and radiological signs of inflammation and complaints from patients indicated the achievement of a positive treatment result. At the moment of observation, the patients’ condition is stable, which suggests the high efficiency and predictability of this technique.
Clinical observations
Patient K., born in 1982, applied to the maxillofacial surgery department of the State Medical Hospital No. 2 in August 2009 with complaints of pain in the area of the 21st and 22nd teeth.
Objectively: there were restorations in the area of 21 and 22 teeth. Localized swelling and hyperemia of the gingival margin and degree I tooth mobility were observed. An orthopantomogram and a dental volumetric computer image (Morita) revealed a periapical lesion with clear boundaries measuring 12.74 mm. In 2005, the patient underwent resection of the apical roots at another institution (Fig. 1 a, b).
Rice. 1a. Odontogenic cyst in the area of the 21st, 22nd teeth. Relapse after a previous apicotomy. Sight X-ray.
Rice. 1b. View of the cyst on a dental volumetric computed tomography section.
Diagnosis: odontogenic cyst of 21, 22 teeth.
Treatment: cystectomy, repeated RVC, retrograde filling of teeth 21 and 22 with MTA, filling of the bone defect with osteoplastic material.
3 months after the operation, the process of bone tissue restoration is observed on the orthopantomogram (Fig. 1c).
Rice. 1st century Condition of tissues 3 months after surgery. Orthopantomogram.
After 12 months, the patient’s condition is stable, she has no complaints, there is no tooth mobility, and there are no signs of inflammation in the periradicular tissues.
On a dental volumetric computer image (Morita) after 12 months, restoration of periapical tissues and the formation of a periodontal gap in the MTA area were observed (Fig. 1d, e).
Rice. 1 year Condition of tissues 12 months after surgery on a section of dental volumetric computed tomography (area of the 21st tooth).
Rice. 1d. Condition of tissues 12 months after surgery on a section of dental volumetric computed tomography (area of the 22nd tooth).
When choosing a treatment method, the patient’s wishes to try to save her teeth and delay the time of subsequent implantation were taken into account.
Conclusion
Improvements in the surgical method of treating periradicular pathology have influenced the attitude of specialists and patients to this type of treatment. Thus, the changes that have occurred over the past 10 years in the field of endodontic surgery suggest its effectiveness and predictability of this type of treatment. Periapical surgery is not a substitute for quality conservative root canal treatment. Conservative treatment should be carried out first, ensuring the opportunity to avoid surgical intervention.
Surgical treatment is used to overcome the following problems: removal of pathologically changed periapical tissues when conservative treatment is difficult or impossible, performing a biopsy, as well as correcting iatrogenic errors. The use of microsurgical instruments, retrograde preparation with ultrasonic tips and retrograde filling with biocompatible materials, filling of the bone defect with osteoplastic preparations during surgery allows us to speak about a high degree of reduction of the pathological focus, restoration of the tissues of the periapical zone and the functionality of the tooth.
Despite the fact that in recent years implantation has become a more fashionable trend than tooth-preserving treatments, we should not forget that one of the main goals of dentistry is to preserve the healthy and natural dental system of patients [12]. “The high success rate in solving endodontic situations, combined with the high success rate of endodontic surgery, allows the preservation of almost all teeth with endodontic problems” (Kim S., JOE, 2006).
Preparation for retrograde tooth root filling
Before prescribing retrograde filling to a patient, CELT dentists conduct a full diagnostic study. It is indicated for microsurgical intervention and includes:
- Thorough dental examination;
- Sight radiography/panoramic photo;
- Test for individual intolerance to filling materials.
If there are no contraindications to filling, the dentist performs sanitation of the oral cavity, after which the patient is ready for intervention.
Clinical application of collagen and hydroxyapatite granules in filling bone defects
| Before treatment. There are extensive bone defects. | At the stage of surgical intervention. The defects are filled with granules of osteoplastic material. |
| Treatment result after 3 months. Partial osseointegration occurs as the graft material is absorbed. |
Principles of retrograde filling of the reserved root canal
It is carried out in several stages, which are as follows:
- Infiltration anesthesia - local anesthesia with the introduction of an anesthetic with a syringe into the soft tissue of the gums;
- Providing access to the apex of the root of a dental unit - an incision along the gum and peeling off its mucous membrane exposing the bone jaw tissue and excision of the apex of the root to the level of detection of the canals;
- Antiseptic treatment - the cavity remaining after excision is cleaned, removing fragments of pathological tissue from it (if any), filling it with tampons with an antiseptic;
- Preparation for retrograde filling - the apex is thoroughly dried and etched, after which the cavity is washed and also dried;
- Retrograde filling - the canal cavities are filled with filling materials, covered with tampons for five minutes to harden, after which antiseptic treatment is carried out and excess composition is removed;
- Suturing - the detached flap of gum is returned to its place and secured with sutures. During the first 48 hours after surgery, drainage will be required to drain the ichor.
General overview
The retrograde filling method is an alternative to the standard root canal therapy method. The procedure is carried out to prevent the penetration of pathogenic microorganisms into the periapical region through the dental canals.
This technique allows for reliable closure of the apical region. The principle of manipulation is to perform an apiectomy (surgical resection of the tooth root in the apical zone). After preparing the canal, treatment is carried out, and then it is closed with filling material.
Recovery period after retrograde canal filling
The sutures are removed no earlier than after five days. During the recovery period, the patient must follow the doctor’s recommendations, which are as follows:
- During the first half hour, apply an ice compress to reduce swelling;
- Avoid consuming food or liquid for the first two hours;
- Avoid any physical activity for 24 hours;
- Carry out hygiene procedures regularly, but use a toothbrush with soft bristles;
- Systematically rinse the mouth with decoctions of chamomile and sage;
- Take antibiotics and stimulants according to the regimen prescribed by your doctor.
You can make an appointment with CELT dental surgeons online on our website or by contacting our information line operators.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Reviews
Retrograde dental canal filling is a procedure aimed at preserving your teeth.
The newest implantation will not replace the functionality of your own teeth, although they are already dead.
If you have a desire, then share your impressions of this method of treating and preserving teeth.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags: toothache, filling
Did you like the article? stay tuned
Previous article
Oroantral communication - concept and closure techniques
Next article
What are the dangers of inflammation of the gingival papillae, and how to prevent complications?
Retrograde canal filling - what is it?
The operation is performed to prevent pathogenic microflora from entering the periapical area. Essentially, this is an alternative to traditional treatment, but through access to the root system in the gum. The technique is based on resection of the upper part of the root followed by filling.
There may or may not be inflammation or destruction in this area. In the first case, patients complain of pain, swelling of the gums, and the presence of fistulas. In the second case, the problem is more often detected by chance using an x-ray, which is taken to examine adjacent dental units.