Stages of rehabilitation
Carrying out mammoplasty is a fairly serious surgical intervention, performed under general anesthesia, accompanied by tissue incisions and trauma when placing implants, followed by suturing. Therefore, the rehabilitation process takes place in stages, with certain restrictions and prohibitions over several days or weeks. The patient needs to strictly monitor her general well-being, monitor the condition of the postoperative scar and follow all the recommendations of the plastic surgeon. This is necessary so that expectations regarding the desired shape and size of the breast are met, and the recovery process goes according to plan.
In general, the first (postoperative) rehabilitation period lasts up to two months, full recovery occurs within 6-12 months.
Rehabilitation after mammoplasty by day
The patient spends the first day after the operation in the ward under the supervision of a doctor and nurses, recovering from anesthesia. An increase in temperature is possible as a reaction to incisions and tissue injury, pain. Antipyretics, painkillers, and antibiotics may be recommended to prevent wound infection. After the operation, a semi-lying or sitting position is required; by the end of the day you can stand up and walk. You can drink 3-4 hours after anesthesia, eat food after 5-6 hours.
On the second day, the doctor conducts an examination, removes drainages and makes dressings. In some clinics, the patient is allowed to go home by the end of the second or third day with positive dynamics of recovery.
The patient remains at home for the third or fourth day. Physical activity is prohibited; walking around the house is acceptable.
On the fifth day, a visit to the clinic is required for a follow-up examination by a surgeon and assessment of the recovery process, dressing, and suture treatment.
From 6 to 11 days after surgery, there is a smooth return to normal life with a number of restrictions. Physical activity, sports and heavy lifting are prohibited.
On the 12th day, the doctor conducts an examination again, monitoring the process of restoration of breast tissue and postoperative suture. The next visit during the normal rehabilitation process is planned for the 6th week from the date of surgery.
In the second or third week after the intervention, light housework is allowed; after the doctor’s permission, you can start training after about a month.
When is trocar cystomy necessary?
Diseases of the urinary system cause people not only physical suffering and psychological discomfort, but also threaten life. Therefore, surgical treatment prescribed by a qualified doctor is the only correct option.
Trocar cystostomy is prescribed in the following cases:
- prostate adenoma and complications caused by it;
- neoplasms in the genitourinary system;
- abnormal structure of the genital organs;
- stones and rocky formations in the urinary canals, obstructing the outflow of urine;
- mechanical damage to the urethra due to injury to the penis;
- uncontrolled urination caused by psychological problems;
- abdominal surgeries, etc.
A cystoma is installed in cases where the patient, for a number of reasons, is unable to use a traditional catheter.
Bladder surgeries are performed in hospitals and medical centers. After the procedure, the patient, depending on his condition, is transferred to the intensive care ward or to the department ward, where he requires constant care and observation.
Dynamics of changes in the breast during the recovery period
In the first month after surgery, the breasts are quite painful, the tissues swell, and the breast size may be larger than expected. Bruising and small hematomas may appear in the area of the mammary glands. Women are concerned about how long breast swelling lasts after surgery. Maximum swelling will occur in the first week; within 2-3 weeks all these changes will subside. The pain will be maximum in the first days; painkillers are used to eliminate it. Gradually, the intensity of pain decreases by 2-3 weeks, and the need for medications disappears.
In the first two months, the breasts will be somewhat unnaturally raised; by the end of the second month, the implants will completely take root, take their proper place, tissue swelling will go away, and the shape of the breast will become natural. Breast tissue restoration takes place throughout the first year after the intervention. There may be problems with sensitivity of the halos and nipple, burning or itching of the skin. These problems are acceptable and disappear by the end of the first or beginning of the second year.
Diet for trocar cystostomy
People who have cystostomy drainage installed must follow a diet and refrain from eating a number of foods. Meals should be regular and leisurely. During the first time after the operation, this is monitored by a caregiver - a relative or a visiting nurse.
It is not recommended to include fried and smoked, fatty meat, mushrooms, sausages, canned food, as well as marinades and pickles in your diet. You should also exclude dairy products and citrus fruits. The former are rich in calcium, which provokes stone disease, the latter contain oxalic acid, which irritates the mucous membranes of the urinary tract.
Vegetable soups and salads, boiled fish, lean meat, berries, fruits, and herbs are recommended for consumption.
As for drinks, patients with diseases of the genitourinary system should refrain from carbonated water, coffee, strong tea, lemonade, alcohol, and freshly squeezed juices. Herbal and green teas, rosehip decoction, and dried fruit compote will be useful.
Patients need to follow not only a diet, but also a drinking regime. For diseases of the genitourinary system, you should drink at least 1.5-2 liters of liquid per day.
What to pay attention to during the rehabilitation period
There are a number of warning signs, the appearance of which is a reason for immediate consultation with a doctor. The first thing that needs to be monitored is the condition of the postoperative wound and the process of scar formation. It is important to notify your doctor immediately if:
- increased pain in the area of the stitches or inside the chest;
- discharge appeared from the nipple area - green, yellowish, bloody, with an odor;
- the breast is swollen, hard to the touch, painful, sharply increased in size;
- parts of the implant are felt, they move, causing discomfort;
- the sutures become wet and fluid or blood oozes out;
- nipples itch and itch, have lost sensitivity;
- breasts are visually different sizes, asymmetrical.
It is important to monitor your general condition if you feel unwell, have a fever, headache, or nausea. Any signs of malaise, discomfort and other complaints are a reason for an immediate visit to the doctor.
Psychological aspect
People who have undergone cystostomy drainage surgery need sensitive attention and support. For many of them, the operation becomes a psychological shock. Patients may find it difficult to come to terms with the idea that their lifestyle will now change. Many people develop a feeling of inferiority. Often, symptoms of depression are added to the physiological discomfort after surgery.
Therefore, it is very important that there is an understanding person next to the patient during rehabilitation, who is ready not only to ensure hygiene, but also to listen, reassure, and encourage. It is necessary to consistently and calmly convince the patient that life with a cystoma is not a death sentence, but a new stage that gives the opportunity to enjoy the world without pain and suffering.
The patient's relatives and friends, empathizing with him and imbued with his decadent moods, do not always find spiritual strength and the right words to support.
Professional health visitors cope with this much better. Experience in communicating with patients and general training have an impact. If you have the opportunity to choose, then it would be better to entrust the care of your loved one to professionals. In contact with
What not to do after mammoplasty
After the operation, there are a number of restrictions that are gradually weakened as tissues are restored and postoperative scars heal.
You should not drink liquids for the first 3 hours after surgery (vomiting may occur), and you should not eat food for the first 5-6 hours.
For 4-5 days you should not shower your entire body (you can wash your lower part, wipe your hands, neck, and face with a damp towel).
In the first week, you should not lie down, sleep on your stomach at night, raise your arms above shoulder level, lift more than 1 kg of weight, make sudden movements with your arms, or bend forward and down.
Until the end of 2 weeks after the operation, you cannot drive a car or have sex. Until the end of the first year of rehabilitation after mammoplasty, pregnancy is undesirable - you should take care of contraception.
For a month after the operation, physical activity, sports and training are prohibited. Exercises with push-ups and stretching of the pectoral muscles are carried out no earlier than 24-25 weeks after surgery.
During the entire rehabilitation period, you should avoid sudden weight fluctuations, serious stress and nervous strain, and anxiety.
In the first three months, you should stop drinking alcohol and smoking, limit spicy, salty, spiced, fatty and fried foods. It is important to control fluid intake to avoid swelling.
For at least 6 months, you should avoid visiting saunas, steam baths, solariums, prolonged exposure to the sun, and taking hot baths.
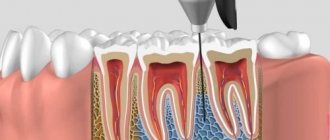
How long can drainage last in the gum?
The drainage structure can be installed for a period of 3 to 6 days. This time is usually sufficient for the complete release of the pathogenic fluid. If after a week the swelling does not disappear, additional examination and a change in medical procedures will be required. This situation may arise after the removal of a wisdom tooth in the upper jaw. The drainage system is removed when the swelling completely subsides, which indicates complete cleansing of the wound area. Now the dentist’s main task is to speed up the healing process.
The doctor determines when to remove the tube or strip. It depends on many circumstances.
- In addition to a visual examination, the dentist may refer the patient for repeat images.
- It is important that yellow and whitish pus, as well as ichor and translucent liquid come out of the wound.
- The patient must close his jaws freely and chew food.
- The redness of the mucous membrane should gradually change to a normal pink color.
The speed of release of pathological fluid is influenced by the patient’s compliance with the doctor’s recommendations. He should eat liquid pureed food, drink enough clean water, and avoid sweets and solid foods.
Important points during the rehabilitation period
In the first days after mammoplasty and subsequent months, proper breast care in the area of postoperative scars is important. This is important for their fastest healing without severe deformations. In the first days, the doctor treats the area of the sutures and changes the bandages; they are prohibited from being removed or wet. If absorbable threads were used, they are not removed; the resulting crust over the seam cannot be torn off until it completely falls off. To stimulate scar healing, your doctor may prescribe special creams. They make the seams less noticeable.
During the first 2-3 months (or longer), you need to wear a compression bra after mammoplasty. For a month they wear it without taking it off, even at night; from the second month it is permissible to take off the underwear at night. This is important so that the implants take their place and take root well, there are no problems with the skin and ligaments, muscles, and blood flow and lymph drainage are normalized.
On the recommendation of a doctor, therapeutic breast massage may be prescribed. Initially, it is carried out by a massage therapist, teaching the woman, then she performs it independently, in the morning. In the first three weeks, movements should be as light as possible, then lymphatic drainage massage techniques are used.
What causes appendicitis?
Appendicitis is an inflammation of the vermiform appendix of the cecum, the appendix. The function of the appendix in the body has not been fully established. It is rather a vestigial organ. It is assumed that in the course of human evolution it has lost its main digestive function and today plays a secondary role:
- contains a large number of lymphoid formations, which means it partially provides immunity;
- produces amylase and lipase, which means it performs a secretory function;
- produces hormones that provide peristalsis, and therefore is akin to hormonal glands.
The causes of appendicitis are described by several theories:
- the mechanical one states that the reason for the development of appendicitis is obstruction of the lumen of the appendix with fecal stones or lymphoid follicles against the background of activation of the intestinal flora; as a result, mucus accumulates in the lumen, microorganisms multiply, the mucous membrane of the appendix becomes inflamed, then vascular thrombosis and necrosis of the walls of the appendix directly occur;
- the infectious theory is based on the fact that inflammation of the appendix is caused by an aggressive effect on the appendix of infectious agents localized here; usually this is typhoid fever, yersiniosis, tuberculosis, parasitic infections, amebiasis, but specific flora has not yet been identified;
- the vascular theory explains the development of appendicitis by a disorder of the blood supply to this part of the digestive tract, which is possible, for example, against the background of systemic vasculitis;
- endocrine The basis for the occurrence of appendicitis is the effect of serotonin, a hormone produced by multiple cells of the diffuse endocrine system located in the appendix and acting as a mediator of inflammation.
Appendicitis often develops against the background of other disorders of the gastrointestinal tract. A high risk of appendicitis is assessed for those individuals who are diagnosed with:
- chronic forms: colitis,
- cholecystitis,
- enteritis,
- adnexitis
Appendicitis most often develops between the ages of 20 and 40; Women suffer from it more often than men. Appendicitis ranks first among surgical diseases of the abdominal organs.
Prevention of appendicitis consists of eliminating negative factors, treating chronic diseases of the abdominal organs, eliminating constipation and maintaining a healthy lifestyle. The diet should include a sufficient amount of plant fiber, since it is this that stimulates intestinal motility, has a laxative effect and reduces the passage time of intestinal contents.