Chewing function and the muscles responsible for it
Without these muscles, we would have to be fed intravenously.
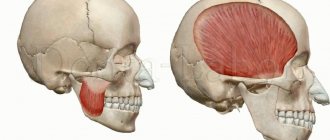
Their well-coordinated teamwork allows us to dig into our favorite burger and enjoy a cold milkshake with appetite. The four main paired muscles of mastication - the masseter proper, medial pterygoid, lateral pterygoid and temporal - are attached to the skull and lower jaw. They are responsible for movements of the temporomandibular joint .
The buccal and mylohyoid muscles play an auxiliary role in the process of eating and drinking.
Muscles of Mastication : These powerful muscles lift your lower jaw so you can close your mouth and chew food.
One of the strongest facial muscles, the masseter muscles are thick, flat, and rectangular in shape and are attached to the lower jaw and cheek bones on either side of the face.
Medial pterygoid muscles : these muscles have three functions.
Being also located on both sides of the head, they work as follows:
- With the simultaneous contraction of both muscles, the lower jaw moves forward.
- Contraction of one medial pterygoid muscle leads to movement of the jaw in the opposite direction - this is how we move the jaw left and right.
- Thanks to the simultaneous work of the medial pterygoid, masticatory and temporal muscles, we are able to close our mouth and bite.
These muscles are attached to the pterygoid processes of the sphenoid bones of the skull and the inner surface of the angles of the lower jaw.
Lateral pterygoid muscles: the work of these muscles is no less important - they are responsible for opening the mouth, and after you bite off a piece of, for example, pie, they help chew it.
These short, wing-like muscles are located above the medial pterygoid muscles on either side of the head.
Temporalis muscles: The temporalis muscles, which look like large fans, are located, as you might guess, at the temples and help close the mouth.
Cheek muscles: we don’t bite our cheeks when chewing food This is due to the fact that the cheek muscles keep them at a safe distance from the teeth.
You can understand where the cheek muscle is located by touching with your fingers the depression on the inside of the cheek between the upper and lower jaws.
The cheek muscles have three functions, two of which are not related to mastication:
- Helps you avoid biting your cheeks while eating.
- They control the movement of air flow in the oral cavity when whistling, inhaling and exhaling, which is necessary for normalizing breathing and playing wind musical instruments.
- Together with other muscles, they help us smile.
Mylohyoid muscles : swallowing movements play an important role not only in nutrition, but also in the act of articulate speech. When you swallow, a pair of mylohyoid muscles help raise the floor of your mouth, making this action easier.
Correction of bite by treatment of dysfunction of the temporomandibular joint
We usually don't think about how our jaw moves. When most people talk about bite, they mean teeth. But, as mentioned above, the bite is an entire system that controls the position of the jaw. Here are its components and their role:
The role of muscles
Figure No. 4 Opening, closing the mouth, chewing and swallowing occurs due to the work of a large number of muscles.
The opening of the mouth is ensured by the muscles located in the neck. The muscles that support the mandible are located behind the jaw and run under the cheeks to the frontal and postauricular areas.
The most powerful muscles responsible for chewing are located in the cheek area.
Figure No. 5 Our body strives to carry out all functions with the greatest rationality and the least amount of energy. Therefore, normally, the chewing muscles hold the jaw in a position in which the teeth are separated by 1-2 mm.
Figure No. 6 From this rational position, the lower jaw moves hundreds of times a day until the teeth close to swallow.
All this happens subconsciously. Our brains are hardwired for a process called proprioception.
With proper bite and jaw position at rest, most muscles are in a relaxed state.
If your teeth don't close quite correctly, your muscles can adjust, causing your jaw to close in a pattern that causes excessive tension, spasm, and muscle fatigue over time.
In this case, the position of physiological rest of the lower jaw (when the teeth are not closed) is not accompanied by muscle relaxation, as it should be with normal occlusion, but, on the contrary, leads to their constant tension.
The role of joints
Figure No. 7 The lower jaw moves thanks to the joints. called the temporomandibular joints, or TMJs.
Think of the joint as a ball in a basket - the articular head (ball) moves in the recess of the skull (basket). Between them there is a soft tissue layer (articular disc).
The position of the articular head (condyle) in the corresponding depression of the skull (fossa) is largely determined by the bite (occlusion) - the position where the muscles hold the jaw.
Figure No. 8 If the system is balanced, the condyles are located in the center of the glenoid fossa and the disc, located between the articular head and the glenoid fossa, moves freely in the joint when opening and closing the mouth.
Figure No. 9 If the masticatory muscles adapt to the incorrect position of the jaw, they can hold the head of the joint in a displaced position, negatively affecting its function. This often causes the articular disc to become dislodged, preventing it from moving normally in the joint until it moves completely into its normal position when the mouth opens. When this happens, a clicking sound occurs.
The intensity of the click can vary from a barely perceptible vibration to a very loud sound.
This sound is often a sign of abnormal joint function, which in turn may be associated with a malocclusion.
The role of posture
Posture also plays a significant role in occlusion. The mandible and lower limbs can be considered interdependent parts of the human skeletal system. If any of these parts are negatively affected, other parts of the skeleton may be affected.
Let's check this by slightly closing our teeth. Pay attention to which teeth closed first. Then tilt your head back as much as possible and clench your teeth again. Don't be surprised if the first contact is on other teeth this time. By changing the position of your head, you thereby influence the balance of the entire skeletal system (and your bite in particular).
The same thing happens when you get a filling. Lying in the dental chair under anesthesia, it seems that the filling is not in the way. But after the anesthesia wears off and you get up from the chair, you notice that the filling is higher than the rest of your teeth. This is why in neuromuscular dentistry, the bite is assessed in the sitting position - the position in which your jaw is normally located. If you evaluate the bite in a sitting position, leaning back, the jaw also moves posteriorly. This situation is different from the usual one.
Photo No. 10,11 In an experiment on rats, an oversized filling was made on one lateral tooth on the right side. A week later, an x-ray examination revealed deformation of the entire spine. After leveling the occlusion by making a filling on the lateral tooth on the left, the shape of the spine was restored.
Figure 12 Since there is a direct connection between all parts of the musculoskeletal system, head position undoubtedly affects occlusion, and can cause tension in the neck and back muscles. Figure No. 13 When the lower jaw moves back as a result of malocclusion in childhood or wear of teeth over time, the neck moves forward and the head is thrown back. This, in turn, significantly increases the load on the muscles of the neck and shoulder girdle. Therefore, most people with an anterior head position experience neck pain or neck muscle tension. Figure No. 14, 15 Often, displacement of the lower jaw due to malocclusion is accompanied by rotation of the first and second cervical vertebrae, which leads to severe deformation of the entire cervical spine.
Just as changes in jaw position can cause changes in posture and lead to pathology in the cervical spine, changes in the spine can affect jaw position and occlusion.
The role of breathing and sleep apnea
Figure No. 16 Displacement of the lower jaw back often leads to a narrowing of the airway due to deformation of the cervical spine and posterior displacement of the tongue, which follows the lower jaw. In order to increase the clearance of the airways, the muscles move the neck further forward and tilt the head back.
In this case, the artery that carries blood to the brain along the spine can sharply bend in the area of the first and second cervical vertebrae, causing disturbances in the blood supply to the brain.
Narrowing of the airways and impaired blood supply can cause sleep apnea - a short-term cessation of breathing during sleep.
Repeated stops in breathing lead to a significant change in the metabolism of the entire body and, as a result, can become one of the triggers for diseases such as hypertension, diabetes, myocardial infarction, stroke, etc. Therefore, the untreated condition of sleep apnea is responsible for reducing life expectancy by 20%.
Now you understand that occlusion is much more complex than just the way the teeth are closed! And malocclusion can cause not only early tooth loss, but also cause serious pathologies such as diabetes and myocardial infarction and even reduce life expectancy.
Facial muscles.
The facial muscles are closely intertwined and are located around the eyes, nose, ears, and mouth. The facial muscles include the muscles of facial expression and mastication, which are attached to the skin and soft tissues of the face. The overall structure includes about 20 flat skeletal muscles lying under the skin of the face and scalp. All of them, with the exception of the buccal, are not surrounded by fascia.
The structural features allow the facial muscles to move the skin and soft tissues relative to the bony surface of the skull. This contributes to the formation of furrows, folds, wrinkles and dimples, which change facial expression and play a big role in matters of appearance. The facial muscles are connected to the nervus facialis—the facial nerve. When the facial nerve is damaged and inflamed, the corresponding muscles partially or completely lose their functions and do not work properly, which leads to visible changes in appearance.
Chewing group of facial muscles.
It provides the chewing process. Consists of the temporal - temporalis, chewing - masseter, lateral and medial pterygoid muscles.
The temporal lobe, accordingly, is located in the temporal fossa. The lateral and medial pterygoids are in the infratemporal fossa. The chewing muscle is located in the cheek area. The muscles of this group are attached to the lower jaw and are responsible for its movement in the temporomandibular joint during functions such as chewing and grinding.
Mimic group of facial muscles.
Most facial muscles contribute to the expression of emotions. The consequence of contraction of the muscles of this group is a change in facial expression.
Accordingly, the more often the facial muscles are involved, the higher the likelihood of premature wrinkles appearing on the face and neck, since the cervical and facial muscles are closely connected. A distinctive feature is that the muscles in this group are relatively thin and are attached directly to the skin, connecting to each other in separate bundles.
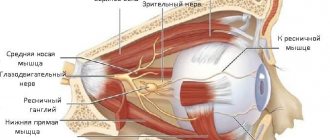
Muscles of the eye circumference.
- The orbicularis oculi muscle consists of several parts: orbital, secular, lacrimal.
- The orbital muscle is responsible for closing the palpebral fissure, forming folds in the orbital area and transverse wrinkles in the frontal part.
- The century muscle is responsible for closing the eyelids.
- Lacrimal muscle - expansion of the lacrimal sac, filling with tear fluid.
- The corrugator muscle is responsible for bringing the eyebrows closer together and takes part in the formation of interbrow folds.
- The proud muscle is responsible for the middle part of the eyebrows and wrinkles the skin between the eyebrows.
- The depressor brow muscle lowers the eyebrow and promotes the formation of transverse folds in the area of the root of the nose.
Muscles of the mouth circumference.
The muscles of the mouth belong to the buccolabial group and are a complex structural unit. The main functions are to control the movements of the lips and mouth. In total, there are 2 main categories of muscles in this group, which have different functional purposes: squeezing, raising and extending the lips, lowering the corners of the mouth, and others.
The functions performed by the muscles around the mouth correspond to the name.
- Orbicularis oris muscle
- Greater zygomatic
- Zygomatic minor
- Laughter muscle
- Depressor muscle - depressor anguli oris
- Lowering lower lip
- Elevator of the upper lip
- Raising the corner of the mouth
- Mentalis muscle
- Transverse chin muscle
Muscles of the nasal circumference
The nasal muscle begins in the upper jaw, attaches to the nasal bone and is a group of muscles that consists of two parts. The outer one goes around the wing of the nose, then widens slightly at the midline and passes into the tendon. The inner part is attached to the posterior end of the cartilage of the nasal wing.
- The nasalis muscle is responsible for narrowing the nostrils.
- The depressor septum muscle is responsible for widening the nostril at the entrance.
Source: https://bbtape.ru/
Movements of the lower jaw, bite and occlusal contacts of teeth
Opening the mouth. The initial position of the lower jaw when opening the mouth is the state when the lips are closed. At the same time, there is a gap of 2-4 mm between the dentition of the lower and upper jaw. This state is called a state of physiological rest.
The lowering of the lower jaw is carried out under the weight of the bone itself and bilateral contraction of muscles: the jaw - the hyoid muscle, the chin - the hyoid muscle, the anterior belly of the digastric muscle. There are 3 phases in the lowering of the lower jaw - slight, significant and maximum lowering. This corresponds to 3 types of movement of the articular heads.
A slight lowering of the lower jaw (quiet speech, drinking) occurs when its head moves in relation to the disc in the “lower floor” of the temporomandibular joint. In this case, identical movements simultaneously occur in the right and left joints along axes running along the greatest length of the ellipsoidal head of the lower jaw, and the midpoint of the central lower incisors describes an arc about 20 mm long.
With a significant lowering of the lower jaw (loud speech, biting) and hinge rotation in the “lower floor” of the joint, the articular heads, together with the discs, slide forward along the circumference of the articular surface, i.e. movement also occurs in the “upper floor” of the joint.
With the maximum lowering of the lower jaw, the sliding of the heads is delayed at the top of the articular tubercle by the tension of the articular capsules, articular ligaments and muscles. In this case, the midpoint of the lower incisors describes an arc up to 50 mm long.
Further excessive opening of the mouth can also occur with a slight hinge movement of the articular heads, but this is highly undesirable, since there is a danger of stretching of the ligamentous apparatus of the temporomandibular joint, dislocation of the head and disc.
Closing the mouth. Raising the lower jaw is carried out by contracting the muscles that lift the lower jaw (masseter, temporal, medial pterygoid) and the movements occur in the reverse order. The articular heads are displaced back and upward to the base of the slopes of the articular tubercles. The closing of the mouth is completed due to the hinge movements of the articular heads until occlusal contacts appear.
Movement of the lower jaw forward. After reaching the initial contact of the chewing teeth (centric relation), the articular heads move forward and upward - into central occlusion. At the same time, they move 1-2 mm along the midsagittal plane, without lateral displacements, with simultaneous bilateral contact of the slopes of the cusps of the lateral teeth.
The advancement of the lower jaw forward with the teeth closed from the central occlusion to the anterior one is carried out due to the contraction of the external pterygoid muscles on both sides. This movement is guided by the incisors. If the lower incisors in central occlusion are in contact with the palatal surfaces of the upper incisors, moving the lower jaw forward from this position causes disocclusion of the lateral teeth. The sliding continues until the cutting edges of the teeth of the lower jaw come into contact with the cutting edges of the teeth of the upper jaw. The path that the lower incisors take along the palatal surfaces of the upper incisors is the sagittal incisal path, and the angle between this path and the occlusal plane is the angle of the sagittal incisal path. During this movement, the articular heads move forward and down the slopes of the articular tubercles, making a sagittal articular path, and the angle between this path and the occlusal plane is called the angle of the sagittal articular path.
These angles and their individual determination for each patient are used to adjust the articulator - a device that simulates the movement of the lower jaw.
When moving the lower jaw forward between the dentition, contact is maintained at several points: between the incisors, between individual chewing teeth on the left and right sides. The cusps of the last molars of the lower jaw stand above the level of the cusps of other chewing cusps of the first and second molars of the upper jaw below the level of its other chewing teeth. These contacts in the literature are called the three-point Bonville contact or the Bonville triangle point. The sides of the triangle connect the centers of the right and left articular processes of the lower jaw and the incisal point and average 10 cm.
Lack of contact in the area of chewing teeth when biting, when there is occlusal contact on the incisors, can lead to overload of the latter, and with artificial dentition replacing a defect in the front teeth or a complete defect in the dentition (dentitions) - to the overturning of the dentures. This can cause overload of the joint, since the intra-articular disc, moved to the top of the articular tubercle, experiences increased pressure from the articular head, and the capsule and ligaments of the joint are stretched. If a three-point contact (according to Bonneville) is created on artificial dentition, then the pressure on the joint discs is reduced, the ligaments are stretched less, and the fixation of the prosthesis is better.
Lateral movements of the lower jaw
Rice. 10. Scheme of lateral movement of the lower jaw to the left in the horizontal plane (a), possible paths of movement of the head of the balancing side (b) and the “occlusal compass” (c):
A, B - initial position of the jaw;
A1, B1 - position of the jaw when shifted to the left;
B – B1 – Bennett movement;
B is Bennett's angle. The dotted line indicates “initial lateral movement”;
c - “occlusal compass” - a path that describes the supporting palatal cusp of the upper left first molar on the occlusal surface of the lower first molar shown in the figure;
E – forward movement;
G – movement to the left;
D – movement to the right.
During lateral movement of the mandible from the position of central occlusion, the articular head on the side of displacement (side of laterotrusion) rotates around its vertical axis in the corresponding glenoid fossa and makes a lateral movement, which is called Bennett's movement. This lateral movement of the working articular head averages 1 mm. The articular head on the opposite side (the mediotrusion side) moves downwards, forwards and inwards. The angle between this path of head movement and the sagittal plane is Bennett's angle (~ 17º). The greater the Bennett angle, the greater the amplitude of the lateral displacement of the articular head of the balancing side.
With a lateral displacement of the lower jaw, the lateral pterygoid muscle of the side opposite to the displacement of the lower jaw contracts, therefore, with a unilateral type of chewing, unilateral hyperactivity of the muscle can occur, which adversely affects the function and structure of the TMJ, the condition of the hard tissues of the teeth and periodontium.
When studying the structure of the dentition of the lower and upper jaws in the area of chewing teeth, the following was established:
a) the crowns of the chewing teeth of the lower jaw are inclined towards the tongue, resulting in an equal level of location of the buccal and lingual cusps;
b) the palatal cusps of the maxillary molars are located lower than the buccal ones.
As a result of different levels of arrangement of the cusps of the chewing teeth, lateral occlusal curves are formed that pass through the buccal and lingual cusps of both sides of the chewing teeth. Lateral occlusal curves ensure the preservation of occlusal contact in the area of the chewing teeth with a lateral shift of the lower jaw, which is equal to no more than half the width of the chewing teeth.
During lateral movements of the lower jaw, the occlusal relationship between the cusps of the antagonist teeth on the balancing and working sides is different. On the side of the contractile muscles, the antagonists meet with tubercles of the same name (working side), on the opposite side - with opposite tubercles (balancing side).
Literature:
- S. I. Abakarov, ed. E. S. Kalivradzhiyan “Fundamentals of dental prosthetics technology - a textbook for medical schools and colleges. Moscow, 2016. M.: “Geotar – Media”. pp. 130 – 146.
- I.V. Alabin, V.P. Mitrofanenko “Anatomy, physiology and biomechanics of the dental system” - M., “ANMI”, 1998, p. 73-93, 99-114, 178-181.
- Shcherbakov A.S., Gavrilov E.N., Zhulev E.N. “Orthopedic dentistry”, St. Petersburg: IKF “Foliant”, 1998, p. 44-51
Original work:
Movements of the lower jaw, bite and occlusal contacts of teeth
Muscles depressing the lower jaw: - mylohyoid, - geniohyoid, - anterior belly of the digastric muscle. Places of attachment: - Mylohyoid - flat, participates in the formation of the muscular base - the diaphragm of the oral cavity. It starts from the line of the same name of the lower jaw and is attached by posterior bundles to the anterior surface of the body of the hyoid bone, and the main part of the muscle fibers meets the fibers of the muscle of the same name on the opposite side, forming a fibrous suture. Function: Raises the hyoid bone, and when the hyoid bone is fixed, lowers the lower jaw. - Geniohyoid - located above the mylohyoid muscle. It starts from the mental spine of the lower jaw and attaches to the body of the hyoid bone. Function: pulls the hyoid bone up and forward, and when supported by the hyoid bone, lowers the lower jaw. - Anterior belly of the digastric muscle - the anterior belly begins from the digastric fossa of the mandible. It is connected by a tendon to the second belly and is attached to the body and greater horn of the hyoid bone through a dense fused loop. Function: lowers the lower jaw, pulls it back. With a fixed lower jaw, it raises the hyoid bone. Muscles that lift the mandible: - The masticatory muscle itself; - Temporalis muscle; - Medial pterygoid. Places of attachment: - The masticatory itself is rectangular, starts from the lower edge of the zygomatic arch, attaches to the lateral surface of the coronoid process of the mandible, as well as to the masticatory tuberosity of the mandible. Function: raises the lower jaw. — The temporal jaw is wide, fan-shaped, and occupies the area of the same name on the lateral surface of the skull. It starts from the temporal surface of the large wing of the sphenoid bone, the squama of the temporal bone. Attached to the apex and medial surface of the coronoid process of the mandible. Function: raises the lower jaw, the anterior fascicles pull the jaw upward to the front, the posterior fascicles pull it back. - Medial pterygoid - starts from the pterygoid fossa of the same process of the sphenoid bone, attaches to the pterygoid tuberosity on the inner surface of the angle of the lower jaw. Function: with unilateral contraction, it moves the jaw in the opposite direction; with bilateral contraction, it moves the jaw forward and lifts it. Muscles that protract the mandible: Paired lateral pterygoid muscle. With their synchronous contraction, the lower jaw moves forward; with unilateral contraction of the muscle, the lower jaw moves in the opposite direction, thus the muscles of the third group provide anterior and lateral movement of the lower jaw. Place of attachment: Located in the inferotemporal fossa. It starts from the infratemporal crest and the maxillary surface of the greater wing of the sphenoid bone, from the lateral plate of the pterygoid process of the same bone: it is attached to the articular capsule of the TMJ, the articular disc, and the anterior surface of the neck of the lower jaw. Function: with unilateral contraction, it shifts the lower jaw to the opposite side, with bilateral contraction, it pushes it forward.You might be interested in:
- Bite
- Central occlusion
- Movements of the lower jaw.
- Strength of masticatory muscles
- Functions of chewing
We recommend reading:
- Dentition
- Mucous membrane.
- Temporomandibular joint (ellipsoidal incongruent, paired, complex). Consists of: - glenoid fossa; - articular head; - articular bu...
"> Temporomandibular joint
- Solid sky
- The upper jaw is a paired bone. Each half has a body and 4 processes: - frontal; - zygomatic; - palatal; - alveolar...
">Structure of the upper jaw
The structure of the neck muscles.
The neck muscles are a large array of superficial, middle and deep muscles. The neck muscles are primarily responsible for tilting and other head movements in all directions. In addition, they perform several other functions: keeping the head in balance, helping with swallowing and pronouncing sounds. The neck muscles are closely connected to a number of important structures and, unlike the facial muscles, are covered with dense fascia.
Superficial muscles of the neck.
The superficial muscle group consists of two parts: the subcutaneous muscle and the sternocleidomastoid muscle.
The sternocleidomastoid muscle is a long splenius muscle with two heads. The muscle originates from the sternal head (the anterior surface of the manubrium of the sternum) and the clavicular head (the upper surface of the middle third of the clavicle). The place of its attachment is the mastoid process of the temple bone, or rather the outer surface of this process.
If both halves contract, the muscle pulls the head forward and bends the neck. When you inhale deeply, it lifts the ribs and sternum up. If one half contracts, the muscle tilts the head forward on the side of contraction. Responsible for rotating the head up and in the opposite direction.
The saphenous muscle is located just under the skin and is flat and thin. It begins in the chest area below the collarbone, passes medially and upward, occupying almost the entire anterolateral area of the neck. Only a small triangle-shaped area located above the jugular notch remains unclosed.
Bundles of the subcutaneous muscle rise into the facial area and are woven into the masticatory fascia. Some of them attach to the laughter muscle and the muscle that depresses the lower lip. This muscle pulls back the skin and protects the veins from compression. It can also pull the corners of the mouth down, which is important for human facial expressions.
Middle or median muscles of the neck.
This muscle group includes: the lateral and medial pterygoid muscles, the buccal muscle, the median, anterior and posterior scalene muscles, the digastric, the thyrohyoid and sternohyoid, the sternothyroid and trapezius muscles.
The mylohyoid muscle has the shape of an irregular triangle and is flat. It begins in the area of the lower jaw, where the mylohyoid line is located. The muscle bundles go from top to bottom, as well as from back to front. Reaching the midline, they connect with the bundles of the same muscle on the opposite side and form a suture of the mylohyoid muscle. The posterior bundles join the anterior portion of the hyoid bone. The left and right mylohyoid muscles form the floor of the mouth and are called the diaphragm of the mouth.
The main task of the mylohyoid muscle is to lift the hyoid bone upward. If the muscle is fixed, it helps lower the movable (lower) jaw and is an antagonist of the masticatory muscles. When the muscle contracts while eating, it lifts and presses the tongue against the roof of the mouth, allowing the bolus of food to pass into the throat.
The digastric muscle is the tendon that connects the posterior and anterior belly and is attached to the greater horn and body of the hyoid bone using a fascial loop.
The digastric muscle helps with active opening of the mouth (with resistance, for example), lowering the lower jaw while the hyoid bone is fixed.
When swallowing, it lifts the hyoid bone to the mastoid process and the lower jaw (if the latter is fixed by the masticatory muscles).
The stylohyoid muscle has a thin, flattened belly, starting in the area of the styloid process of the temporal bone, running forward and downward, located along the digastric muscle (the anterior surface of its posterior abdomen). The distal end of the muscle splits, covers the tendon of the digastric muscle with legs, attaches to the greater horn, the body of the hyoid bone and plays an important role in the process of articulate speech.
The sternohyoid muscle is located deep. The function of the muscle is to lower the hyoid bone. When the suprahyoid muscles (located between the mobile jaw and the hyoid bone) contract, the sternohyoid muscle, together with the maxillary and sternothyroid muscles, moves the lower jaw.
The geniohyoid muscle begins in the area of the mental axis of the lower jaw, then goes down and back. Located above the mylohyoid muscle, it is attached to the body of the hyoid bone (its anterior surface).
Raises the hyoid bone upward. To a fixed state, it helps to lower the movable jaw, which makes it an antagonist of the masticatory muscles.
The scapulohyoid muscle is part of the subhyoid muscle group and is a paired muscle on the anterior surface of the neck. It has a long, flattened shape and a tendon that divides it into two abdomens. It pulls down the hyoid bone and provides tension on the pretracheal plate of the cervical fascia.
The sternothyroid muscle has a flat shape. It originates from the posterior surface of the first cartilage and the manubrium of the sternum, goes upward and attaches to the thyroid cartilage of the larynx (an oblique line of its lateral surface). The main task of this muscle is to lower the larynx.
The thyrohyoid muscle starts from the oblique line of the thyroid cartilage. Attached to the greater horn, the body of the hyoid bone. Raises the larynx with the hyoid bone fixed.
Deep muscles of the neck.
The deep neck muscles are a complex of lateral and medial (prevertebral) muscles. The list of deep tissues includes the anterior, posterior, middle scalene, longus colli, lateral rectus, anterior rectus and longus capitis muscles.
The anterior scalene muscle originates from the anterior tubercles of the third and fourth cervical vertebrae, goes down and forward, and is attached to the anterior scalene muscle of the first rib in front of the groove of the subclavian artery.
This muscle plays an important role in the functioning of the body. It ensures the elevation of the upper rib during breathing, rotation of the neck in different directions, and forward bending of the cervical portion of the spinal column.
The middle scalene muscle begins in the region of the posterior tubercles of the six lower vertebrae of the neck, goes down behind the anterior scalene muscle and is attached to the upper surface of the 1st rib, behind the groove of the subclavian artery.
The middle scalene muscle acts as an inspiratory muscle (raises the first upper rib). With fixed ribs, it contracts on both sides and bends the cervical part of the spinal column forward. With a unilateral contraction, it bends the same part of the spine and turns it to the left or right.
The posterior scalene muscle originates from the transverse processes of the 6th, 5th, 4th and 3rd cervical vertebrae, moves down behind the middle scalene muscle, and is attached to the outer surface of the second rib.
The posterior scalene muscle acts as an inspiratory muscle. With fixed ribs, it bends the cervical spine anteriorly (since it contracts on both sides). With unilateral contraction, it bends and turns this section in a certain direction.
The longus colli muscle occupies the entire anterolateral surface of the vertebral bodies, from the atlas to the 3rd and 4th thoracic vertebrae. The middle sections of the muscle are slightly expanded. The length of the muscle bundles varies, so the muscle is usually divided into three parts: superior oblique, medial vertical, inferior oblique.
The longus capitis muscle is located in front of the longus colli muscle. The origin is the transverse processes of the 3rd to 6th cervical vertebrae. The place of attachment is the occipital bone (the muscle is located in front of the foramen magnum of this bone). The function of the longus muscle is to tilt the head and flex the upper half of the cervical spine.
The anterior rectus capitis muscle is short. It begins where the lateral mass of the atlas and the anterior surface of the transverse process are located. From here the muscle goes up and is attached to the bottom of the basilar part of the occipital bone, in front of the foramen magnum. The task of the muscle is to tilt the head to one side or another (unilateral contraction) or tilt the head forward (bilateral contraction).
The origin of the lateral rectus capitis muscle is the anterior part of the transverse process of the atlas. From here the beams are directed outward and upward. The muscle ends in the area of the paramastoid process of the jugular process of the occipital bone. The function of the lateral rectus muscle depends on the type of contraction. With unilateral contraction, it tilts the head to the side, and with bilateral contraction, it tilts forward.
Medical Internet conferences
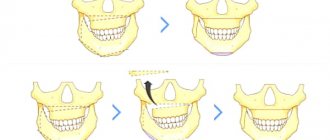
Distal occlusion of the dentition ranks first among pathologies of the dental system. It accounts for 12.4 to 65% of cases of all occlusion anomalies in adolescents and adults. The number of adult patients with this pathology seeking orthodontic care is constantly growing.
Various deformations of the dentition, with distal occlusion, are always accompanied by functional overload of the teeth, dysfunction of the temporomandibular joint and affect the functional state of the muscles of the maxillofacial area.
Functional disorders with distal occlusion of the dentition are detected in 63% - 89% of the examined patients.
In patients with distal occlusion of the dentition, increased tension in the buccal, facial and mental muscles and weakening of the orbicularis oris muscle were revealed.
These functional changes in the muscular system are observed when distal occlusion is formed. Meanwhile, as the cause of the development of distal occlusion, in addition to genetic features of development, the role of disturbances in the activity of the muscular system, leading to secondary deformations in bone structures, is considered. The fact is that the facial muscles can have a dual effect on jaw growth. First, bone formation at muscle insertions depends on muscle activity; secondly, muscles are an important part of the entire tissue base, the growth of which usually moves the jaws.
Most often, changes in the muscles of the maxillofacial area are caused by long-term, incorrectly performed function. Violation of the distribution of chewing pressure leads to structural changes in the supporting apparatus, deformation of the dentition, and occlusion. Moreover, in some muscle groups there is hyperfunction, and in others hypofunction, which causes significant changes in both those and others in the form of compensatory-adaptive deformation, characterized by a restructuring of the fiber composition (the ratio of phasic and tonic muscle fibers), metabolism and contractile properties. It is well known that the adaptive result of increased work is hypertrophy of muscle fibers, while hypofunction is accompanied by a decrease in muscle mass - atrophy.
It is also believed that functional disorders in the form of disturbances in myodynamic balance in the maxillofacial region play a significant role in the formation of distal occlusion of the dentition. Functional disorders are one of the most important reasons for the development of dental anomalies and deformities.
The purpose of the study is to improve the diagnosis of muscle disorders in patients with distal occlusion of the dentition.
Material and methods of the study: 70 people of both sexes aged 15-18 years were examined and 2 age groups were identified: with physiological occlusion (FO) (35 people) and distal occlusion of the dentition (DO) (35 patients).
The type of occlusion of the dentition was determined when they were closed in the usual position of the lower jaw. In patients with DO, during a clinical examination, a violation of the closure of the first molars and the frontal group of teeth was observed (the sagittal incisive gap was 3.0 ± 0.5 mm).
Anthropometric and X-ray (TRG in lateral projection) studies were performed.
Using the method of surface electromyography, biopotentials (BP) were studied in the group of muscles that lift the mandible - the anterior parts of the right and left temporal (Vp and Vl), the right and left muscles of mastication (Zh and Zl), in the muscles that depress the mandible - the right and left suprahyoid muscles ( NPp and NPl) and in the cervical muscles, balancing the position of the head on the spinal column ensuring the position of the lower jaw at rest - the right and left sternocleidomastoid muscles (Sp and GL). Registration was carried out using a computerized electromyograph “Electromyograph BKN” manufactured by Biotronic (Italy).
The bioelectric signal from the muscle, through electrodes, was transmitted to a computer, where it was amplified, purified, and visualized on the monitor screen in real time using the KEY-NET computer program according to specified programs (functional tests).
During the electromyographic study, the following functional tests were used:
Test 1: State of relative rest of the lower jaw (dentitions are not closed, lips slightly touching).
Test 2: State of physiological occlusion of the dentition (primary contact of pairs of antagonist teeth, closure of teeth without load).
An analysis of the amplitude values of biopotentials (BP) was carried out, where two main digital systems for calculating average amplitude indicators of BP are used - ARV and RMS.
In addition to recording and analyzing the average amplitudes of BP of muscles calculated in the RMS and ARV systems, the following indicators were analyzed: total BP of the studied muscles of the right side; average biopotential of the studied muscles on the right (SBP) (sum of BP indicators of the right temporal, masticatory, suprahyoid and sternocleidomastoid muscles divided by 4) or on the left (sum of BP indicators of the right temporal, masticatory, suprahyoid and sternocleidomastoid muscles divided by 4); total biopotential (GBP) (µV) - the sum of all BP indicators of the muscles of the right and left sides; percentage expression of the BP of each studied muscle in the RBP (according to ARV (%) and RMS (%); indicator of the maximum amplitude of biopotentials (MAX) (μV).
Research results:
When studying the biopotentials of the muscles of the maxillofacial area in both digital calculation systems - ARV and RMS, no statistically significant differences were found between the indicators of identical muscles. The RMS and ARV systems have equal capabilities in assessing the functional state of the muscles of the maxillofacial area. Therefore, the RMS calculation system was randomly selected for further research.
1. Persons with physiological occlusion of the dentition
1.1. Relative rest of the lower jaw .
In a state of relative rest, the values of biopotential (BP) indicators of the temporal and masticatory muscles of the right side are higher than those of the left. In the group of muscles depressing the mandible and in the sternocleidomastoid muscles, the digital values on the left side were slightly higher than on the right. There is a “cross” asymmetry in the BP parameters of the maxillofacial muscles (Table 1).
It should be noted that 90% of the examined patients had a predominantly right-sided type of chewing.
However, when comparing the indicator of the own biopotentials of all muscles of the right side (Vp+Zhl+NPp+GKp) (2.3±0.5 μV) with the indicator of the own biopotentials of all muscles of the left side (Vl+Jl+NPl+GKl) (2.0 ±0.2 µV) no significant differences were found, which indicates the myodynamic balance of the muscles of the maxillofacial area.
Expressed as a percentage, the biopotentials of the muscles that lift the mandible on the right side are greater than on the left. In the muscles depressing the mandible and in the sternocleidomastoid muscles, a significant predominance of the muscles of the left side over the right was observed.
The percentages of the levator and depressor mandibular muscles were also compared. A larger percentage of the total bioelectrical activity (TBA) is contributed by the muscles that elevate the lower jaw - 58%, than the muscles that lower it - 16%. 26% were the sternocleidomastoid muscles (Table 1).
1.2. Physiological occlusion of the dentition (habitual closure).
With the usual closure of the dentition, in the muscles that elevate the mandible, the BP of the muscles on the right side predominates, and in the muscles that depress the mandible, the BP on the left side predominates.
In the sternocleidomastoid muscles, BP indices on the left are 1.4 times higher than those on the right (Table 2).
When comparing the BP indices of all the studied muscles during closure of the dentition with the BP indices of identical muscles with relative rest of the lower jaw, no significant differences were revealed in any of them.
Expressed as a percentage, in relation to the total biopotential (TBP) of the studied muscles, the BP of the right temporal and masticatory muscles is significantly greater than that of the left ones. In the muscles depressing the mandible and in the sternocleidomastoid muscles, the percentage of PD on the left is greater than on the right.
The percentage of BP of the mandibular levator muscles on the right side is higher than on the left. The percentage of PD of the right and left temporal and masticatory muscles was 60%. The percentage of PD of the muscles depressing the mandible on the right side is lower than on the left. The percentage of PD of these muscles was 16% (Table 2).
When comparing the indicated indicators when closing the dentition with the corresponding indicators during physiological occlusion, no statistically significant differences were identified for any of them.
Differences in the maximum amplitude of the BP in the temporalis, masseter, suprahyoid and sternocleidomastoid muscles were statistically insignificant between the right and left sides.
2. Patients with distal occlusion of the dentition.
2.1. Relative rest of the lower jaw.
It was found that the BP of the temporal and masticatory, suprahyoid and sternocleidomastoid muscles turned out to be absolutely equal on the right and left.
BP indices in patients with distal occlusion had higher values than BP indices of similar muscles in individuals with physiological occlusion, with the exception of the right masseter muscle.
The average biopotential (ABP) of the studied muscles on the right and left sides was 2 times higher than these indicators in individuals with physiological occlusion (Table 3).
There were no differences between the percentage of BP of the right and left side in any muscle group, while in individuals with physiological occlusion, a significantly higher percentage of BA was found in the muscles of the levator mandible on the right, and in the depressor muscles on the left.
2.1. Closing of the dentition in patients with distal occlusion.
The values of BP of the muscles that raise and lower the lower jaw when closing the dentition on the right and left did not differ significantly and were significantly higher, in contrast to the indicators recorded in individuals with physiological occlusion, where similar indicators were significantly different from each other. There is an increase in the indicators of BP of the temporal muscles, on the right and on the left, compared with those of the masticatory muscles by 2.6 times and 2.1 times, respectively.
When analyzing the average biopotential (ABP) of the muscles of the right and left sides, values were established that did not differ significantly from each other, but were 1.7 times and 1.8 times higher than the values of the SBP of muscles in persons with physiological occlusion of the dentition (Table 4 ).
Analysis of the percentage of BP showed that there are no differences in the muscles of the same name on the right and left sides. Meanwhile, when comparing these indicators with the indicators in individuals with physiological occlusion and with the indicators of patients with distal occlusion at rest, a significant increase in the percentage of PD of the temporal muscles was established.
Discussion
When conducting surface electromyography in persons 15-18 years old with physiological occlusion of the dentition in a state of relative rest of the lower jaw, the values of the biopotentials of the temporal and masticatory muscles on the right side are higher than on the left. The biopotential values of the suprahyoid and sternocleidomastoid muscles on the left side are higher than on the right. The average biopotential of the muscles on the right side is equal to the average biopotential of the muscles on the left side. The total biopotential (TBP) of all muscles studied is 16.7±0.4 μV. In persons with physiological occlusion of the dentition, the indicators of the biopotentials of the muscles of the maxillofacial region, when the dentitions are closed, do not differ from the indicators of the biopotentials of the muscles under study with relative rest of the lower jaw.
In patients aged 15-18 years with distal occlusion of the dentition, the muscles of the maxillofacial region at rest are in a state of increased bioelectrical activity, which indicates their hypertonicity. The greatest increase in bioelectrical activity develops in the temporal (1.8 times in the right and 2.9 times in the left) and suprahyoid muscles (3.6 times in the right and 2.4 times in the left) compared with the indicators recorded in persons with physiological occlusion. The values of the total biopotential (SBP) of the muscles on the right and left sides and the total biopotential (TBP) of the muscles of the maxillofacial region exceed these indicators in persons with physiological occlusion by 2 times. During the initial contact of pairs of antagonist teeth, the work of the muscles is discoordinated, as indicated by a significant predominance of the biopotential values of the temporal muscles over the masticatory muscles (2.0 times on the right and 1.6 times on the left).
Conclusion
The results of the conducted studies deepen knowledge on the functional state of the muscles of the maxillofacial area in individuals with physiological and distal occlusion of the dentition.
The data obtained make it possible to effectively use, for diagnostic purposes, computerized electromyographs with analysis of indicators of bioelectrical activity of the muscles of the maxillofacial area in one of the systems for calculating average values of biopotentials - RMS or ARV.
Hypertonicity of the masticatory muscles and its correction with BTA for aesthetic problems of the lower half of the face
Soykher M.I., Orlova O.R., Mingazova L.R., Soykher M.G.
The aesthetic appearance of the lower half of the face reflects the morphology of the dental system and the function of the masticatory muscles. In aesthetic medicine, the problems of correction of the lower third of the face remain relevant, despite the accumulated many years of experience. The functional state of the masticatory muscle is associated with the configuration of the lower third of the face and possible asymmetry, which hides a combination of dental and neurological problems that require a detailed examination and adequate treatment of the patient. Some diseases, such as bruxism and oromandibular dystonia, are accompanied by hypertrophy of the masticatory muscles, which occurs as a result of their forced contraction, and the massive lower third of the face becomes an aesthetic manifestation here.
Keywords:
Facial disproportion; hypertrophy of the masticatory muscles; bruxism; oromandibular dystonia; myofascial pain syndrome; botulinum toxin type A
Soykher Marina Ivanovna, candidate of medical sciences, dentist, head. Doctor of the Center for Interdisciplinary Dentistry E-mail
Orlova Olga Ratmirovna, Doctor of Medical Sciences, Professor of the Department of Nervous Diseases of the Faculty of Faculty of Physics, First Moscow State Medical University named after. I. M. Sechenova, President of the MoESBT E-mail
Mingazova Leniza Rifkatovna, candidate of medical sciences, neurologist, employee of the department of nervous diseases of the State Educational Institution of Higher Professional Education MMA named after. I. M. Sechenova E-mail
Soykher Mikhail Grigorievich, candidate of medical sciences, dentist, leading specialist of the Center for Interdisciplinary Dentistry E-mail
INTRODUCTION
“Everything in a person should be beautiful.” Today, more and more people are striving to implement this principle in their own lives <2>. Almost every person pays attention to his appearance, and attaches special importance to how his face looks <3, 4>. Dissatisfaction in this case can become quite a serious problem and affect both the psychosomatic state (causing depression, uncertainty, neuroses...), and professional status, family and personal relationships.
In aesthetic medicine, the problems of correction of the lower third of the face remain relevant, despite the accumulated many years of experience. According to a survey of patients, the main complaint they present is facial disproportion, in particular the “square face” problem. What is meant by the expression “square” (or “trapezoidal”) face?
In domestic and foreign medicine, for a brief answer to this question, they use such characteristics as protruding angles of the lower jaw, hypertrophy of the masticatory muscles themselves, prominent contours of the lower zone of the face, angular contours of the face (prominent mandibular angle, hypertrophy of the masseter, lower facial contour). The contours and shape of the lower half of the face are determined by the relative position of the upper and lower jaws (occlusal relationship), the size and shape of the lower jaw, as well as the condition of the masticatory muscles.
The lower jaw is suspended in space to the fixed bones of the skull with the help of muscles and ligaments. The only support for it is the chewing teeth. It is the teeth that fix the position of the jaw in three mutually perpendicular planes. When the position of the teeth and, accordingly, the dentition changes or their loss, the position of the jaw in space also changes. In most cases, there is a decrease in the lower third of the face, distalization of the bite, with characteristic facial manifestations. There are disturbances in the coordination of the masticatory muscles and temporomandibular joints. The dentition, the geometry of which is normally designed to compensate for the complex biomechanics of the chewing function of the cranial-maxillary system, simultaneously serves as support for the soft tissues of the face, which must be taken into account during the aesthetic rehabilitation of patients.
The four chewing muscles on each side are interconnected genetically (they originate from one branchial arch - the mandibular), morphologically (they are all attached to the lower jaw, which they move during their contractions) and functionally (they perform chewing movements of the lower jaw, which determines their location) .
M. masseter is a chewing muscle that starts from the lower edge of the zygomatic bone and zygomatic arch and is attached to the tuberositas masseterica and to the outer side of the ramus of the lower jaw. It has the shape of an irregular rectangle and consists of a superficial part and a deep part. The strongest muscle in the human body in terms of force generated - on molars it develops a force of up to 72 kg.
M. temporalis is the temporal muscle, with its wide origin it occupies the entire space of the temporal fossa of the skull, reaching at the top to the linea temporalis. The muscle bundles converge in a fan-shaped manner and form a strong tendon, which fits under the zygomatic arch and is attached to the processus coronoideus of the lower jaw.
M. pterygoideus lateralis - lateral pterygoid muscle, starts from the lower surface of the greater wing of the sphenoid bone and from the pterygoid process and is attached to the neck of the condylar process of the mandible, as well as to the capsule and to the discus articularis of the temporomandibular joint.
M. pterygoideus medidlis - medial pterygoid muscle, originates in the fossa pterygoidea of the pterygoid process and is attached to the medial surface of the angle of the mandible, symmetrically m. masseter, to the tuberosity of the same name..
M. masseter, m. temporalis and m. pterygoideus medialis, with the mouth open, pull the lower jaw towards the upper, in other words, they close the mouth.
With the simultaneous contraction of both muscles of the pterygoidei laterales, the lower jaw moves forward. The reverse movement is produced by the most posterior fibers of m. temporalis, running almost horizontally from back to front. If m. pterygoideus lateralis contracts only on one side, then the lower jaw moves to the side, in the direction opposite to the contracting muscle. M. temporalis gives a certain position to the lower jaw during speech, thereby ensuring the articulation of the latter.
The masticatory muscle, in addition to chewing movements, takes part, together with the facial muscles, in the articulation of speech sounds, facial expressions, yawning, and swallowing. We can say that this muscle is in a state of “chronic fitness”. Excessive prolonged activity of the masticatory muscles leads to their hypertrophy, which is characterized by an increase in strength and muscle mass (Fig. 5).
The functional state of the masticatory muscle is associated with the configuration of the lower third of the face and possible asymmetry, which hides a combination of dental and neurological problems that require a detailed examination and adequate treatment of the patient. Some diseases, for example, bruxism and oromandibular dystonia, are accompanied by hypertrophy of the masticatory muscles, which occurs as a result of their forced contraction, and their aesthetic manifestation is a massive lower third of the face <6–10>.
The purpose of the study is to study the relationship between the condition of the masticatory muscles and the aesthetic appearance of the lower half of the face; to evaluate the effectiveness of using the botulinum toxin type A drug "Lantox" in order to reduce hypertonicity and correct hypertrophy of the masticatory muscles under the control of surface electromyography.
MATERIALS AND METHODS
40 patients were examined. The average age is 35 years. In order to understand whether problems of an aesthetic nature are caused by pathological processes in the dental system, we conducted a dental and neurological study, which included:
analysis of anamnestic data; clinical study of the masticatory muscles, muscles of the neck and upper shoulder girdle, and the area of the temporomandibular joint (TMJ);
- occlusiogram, analysis of the static and dynamic organization of occlusion;
- orthopantomogram;
- TMJ tomogram;
- teleradiography (TRG) of the lateral surface of the head with markers;
- photoanalysis (portrait and intraoral photographs);
- axiography;
- functional analysis of jaw models in an articulator;
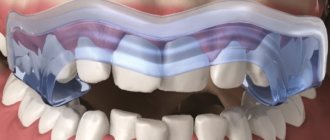
- diagnostics of parafunctions using brookscheckers;
- electromyography (EMG) of the masticatory and neck muscles.
When examining the patient, attention was paid to the following clinical signs: head position, range of active movements in the cervical spine; facial expression, state of the facial muscles when speaking, swallowing, signs of blepharospasm, oromandibular dystonia, facial asymmetry; corneal reflex and reflex from the nasal mucosa, the state of the muscle ridges at rest and when clenching the teeth; volume of active movements of the lower jaw - the distance between the incisors (in cm) when opening the mouth, the trajectory of movement of the lower jaw; mandibular reflex; volume of active movements of facial muscles, brow and orbicular reflexes; Chvostek's sign; sensitivity on the face, oral mucosa and tongue.
Myograph "Synapsis" dental
Electroneuromyograph for maxillofacial studies and monitoring the effectiveness of therapeutic measures.
More details
The study of the state of the musculoskeletal system included: identification of biomechanical static disorders - scoliosis, asymmetry of the shoulders, shoulder blades and other deformities; identification of the “short leg”.
During palpation examination, we used a 3-point scale for assessing muscle tension and soreness:
0 points - no tension and no pain;
1 point - slight muscle tension, no pain on palpation;
2 points - moderate muscle tension and pain on palpation;
3 points - severe muscle tension and sharp pain on palpation, the presence of painful muscle tightness and/or trigger points.
EMG indicators were recorded using an electromyograph “Synapsis” (NMF “Neurotech”, Taganrog), supplemented with special software. Injections of botulinum toxin into the masticatory muscles were carried out under the control of electromyography; for this purpose we used the Mist device (NMF Neurotech, Taganrog).
During the clinical study, 2 groups of participants were identified:
Group 1 - 30 patients who suffered from bruxism: 25 women, 5 men;
Group 2 - 10 patients with signs of focal muscular dystonia (the leading syndrome of oromandibular dystonia): 8 women, 2 (two) men.
"MIST" professional
Myographic control of injections, biofeedback training, anesthesia regimen.
More details
Clinical features
1st group. In dental practice, bruxism is defined as parafunctional activity of the masticatory muscles. The following parafunctions of the masticatory muscles have been described (arranged in descending order of frequency): clenching the teeth, moving the lower jaw forward or to any side, inserting the tongue between the teeth, biting the tongue and lips, grinding the teeth, rhythmic movements of the tongue and submandibular muscles <12–13> . Only 10 patients from group 1 noted grinding and grinding of teeth at night. The rest had the habit of clenching their teeth tightly during the day in response to even minor emotional stress. A hereditary factor (bruxism in close relatives) was determined in all patients in this group. The history also included episodic pain in the face of muscular origin (myofascial pain syndrome of the face), frequent headaches caused by tension in the pericranial muscles. All patients complained of fatigue of the masticatory muscles in the morning. When studying the aesthetic appearance of the face, a massive lower third was determined due to hypertrophy of the masticatory muscles, which caused considerable concern, especially in women.
Dental status in patients of group 1: violation of the integrity of the dentition (absence of one or more teeth), pathological abrasion of teeth, the presence of wedge-shaped defects in the cervical area.
Clinical examination of the masticatory muscles revealed signs of hypertrophy; the muscles are dense, tense, with the presence of painful muscle compactions (myofascial trigger points). When palpating the masticatory muscle itself, in 20 patients the pain radiated to the upper and lower jaws, upper and lower molars, ear, frontal region, TMJ, and neck. In 22 patients, palpation in the area of the tubercle of the upper jaw was sharply painful.
Tenderness or discomfort in the medial pterygoid and digastric muscles was also noted. All patients had muscle tension in the floor of the mouth and limited mobility of the hyoid bone; in 10 patients there was tension and slight hypertrophy of the sternocleidomastoid muscle. Palpation of the muscles on the opposite side was painless or moderately painful.
In 40% of patients, pain occurred on palpation of the lateral pole of the joint head during rotation on both sides, and the temporomandibular ligament on both sides. Discomfort when palpating the lateral pole of the joint head in static conditions on both sides.
In 25% of patients, there was a restriction in mouth opening due to pain to 1.5±2.2 cm between the incisors (normally from 4.6 to 5.6 cm). Further lowering of the lower jaw due to the appearance of sharp pain became almost impossible. There was also a restriction in the movement of the lower jaw forward and to the side.
Only 20% of patients experienced a clicking or crunching sound when opening their mouths. Pain sensitivity of the facial skin and oral mucosa was not changed.
When conducting surface electromyography of the masticatory muscles and neck muscles, the following results were obtained: asymmetry in the work of the temporal, masticatory muscles, high rates of the total biopotential of the muscles under study.
When analyzing a chewing test, a violation of the symmetry of chewing, frequency, amplitude, phase and total biopotential of chewing is noted.
2nd group. Oromandibular dystonia (OMD) is hyperkinesis involving the muscles of the perioral region and masticatory muscles. In patients of group 2, the following clinical forms of OMD were determined: spasm of the muscles that close the mouth and compress the jaw (dystonic trismus) - in 6 people; constant trismus with lateral jerking movements of the lower jaw, bruxism and hypertrophy of the masticatory muscles - in 4 people. Subjectively, all patients of the 2nd group complained of unpleasant sensations, which were described as “periodic movement of the lower jaw”, “the jaw moves to the side”, “it is impossible to find a comfortable position of the jaw”, “forcible clenching of the teeth”, “teeth chattering against each other” friend."
Clinical examination of the masticatory muscles revealed signs of hypertrophy; muscles are dense, tense, with the presence of painful muscle thickening (myofascial trigger points). As a rule, the masticatory muscle itself undergoes pronounced changes, while the temporal and pterygoid muscles undergo smaller changes. Three patients had asymmetric dystonia. Visually, this phenomenon was manifested by asymmetry of the lower half of the face (the volume of the hypertrophied masseter muscle on one side is more pronounced than on the other).
Also, in all patients of group 2, subcompensated signs of dystonic phenomena in other areas were determined: blepharospasm, mild and moderate forms of cervical dystonia, dystonic tremor of the head and upper extremities, writer's cramp.
Dental status: in patients of the 2nd group, there was a violation of the integrity of the dentition (the absence of one or more teeth), pathological abrasion of teeth, and the presence of wedge-shaped defects in the cervical region. When conducting surface electromyography of the masticatory muscles and neck muscles, the following results were obtained: asymmetry in the work of the temporal, masticatory, and neck muscles, torsional twisting of the lower jaw, an increase in the functional activity of the neck muscles and the total biopotential of the muscles under study. When analyzing the chewing sample, a violation of the symmetry of chewing, frequency, amplitude, phase and total biopotential of chewing was noted.
For therapeutic and aesthetic purposes, all patients received injections of botulinum toxin type A (BTA) “Lantox” (Lanzhou Institute, China). It was injected into the masseter proper, temporalis, medial and lateral pterygoid muscles. Large doses were injected into the masticatory muscle itself from the outside (5–10 units at one point). For a more uniform distribution of the drug throughout the muscle, it is injected into several points (from 4 to 8), 1-2 injections are carried out from the oral cavity. In patients with an asymmetric form of dystonia, large doses of the drug were also administered on the side of the larger muscle. The average total dose of BTA (Lantox) was 100 units per procedure.
RESULTS
Analysis of clinical data showed that in patients of group 10 suffering from bruxism, on days 2–10 after injections, the feeling of fatigue in the masticatory muscles in the morning disappeared and headaches stopped. By days 14–21, a decrease in the massiveness of the lower half of the face became noticeable. Against this background, the necessary dental procedures were successfully carried out.
"Hummingbird" dental
Express assessment of the level of bruxism, study of facial muscle tone, wireless technologies.
More details
Due to the weakening of the masticatory muscles, the phenomena of bruxism and the phenomenon of clenched jaws ceased for some time. During this time, patients were advised to fix their attention on the facial muscles, consciously relax the lower jaw, open the dentition and try to form a new motor stereotype of the masticatory muscles (based on the principle of biofeedback). For this purpose, disconnecting splints were used on the lower jaw.
In patients of group 2 (OMD), the signs of hyperkinesis were also leveled out already on days 10–12 after injections due to weakening of the activity of the masticatory muscles, which significantly improved the quality of life of patients. Unpleasant subjective sensations disappeared, and the opportunity for dental treatment appeared. In patients with asymmetric dystonia, the symmetry of the lower half of the face was restored.
The study demonstrated the positive effect of BTA (Lantox) on the functional and morphological state of the masticatory muscles, and a good clinical effect alleviated the condition of patients and made it possible not to use any medications.
CONCLUSIONS
The aesthetic appearance of the lower half of the face reflects the morphology of the dental system and the function of the masticatory muscles. In aesthetic practice, it is necessary to conduct a detailed clinical analysis of the condition of the masticatory muscles, especially in patients with a massive lower half of the face. Patients with increased tooth wear and failing dentures require a detailed neurological examination to exclude bruxism and oromandibular dystonia. Injections of botulinum toxin into the masticatory muscles are the method of choice for this group of patients. The drug botulinum toxin type A (Lantox) at a dose of 100 units per procedure is effective and safe for the treatment of hyperactivity of the masticatory muscles in neurological, dental and aesthetic practice.
LITERATURE
1. Budylina S.M., Degtyareva V.P. Physiology of the maxillofacial region. - M: Medicine, 2001. - P. 87–156.
2. Goldstein R. Aesthetic dentistry. Volume 1. - M.: Stbook. - 2005. - P. 10–14.
3. Kalyuzhny D.V. Physiological mechanisms of regulation of pain sensitivity. - M.: Medicine, 1984. - P. 102–114.
4.Karlov V.A. Neurology of the face. - M.: Medicine, 1991. - 284 p.
5. Kupriyanov V., Stovichek G. Human face. - M.: Medicine, 1988. - 272 p.
6. Mingazova L.R. Pathogenesis and treatment of myofascial pain syndrome of the face // Clinical materials. conference of young scientists FPPO MMA named after. I.M. Sechenov “Current issues of clinical medicine.” - M., 2002. — pp. 54–58.
7. Mingazova L.R. Clinical and physiological analysis and treatment of myofascial pain syndrome of the face. Abstract of thesis. dis…. Ph.D. honey. Sci. - M., 2005. - 25 p.
8.Orlova O.R. Focal dystonia: clinical picture, pathogenesis, treatment using botulinum toxin // Diss.... Dr. med. Sci. - M., 2000. - P. 13–29.
9.Orlova O.R., Mingazova L.R., Vein A.M. Facial pain of a muscular nature: clinical and physiological characteristics and treatment with botulinum toxin type A (dysport) // Abstracts of the Russian scientific and practical conference “Clinical and theoretical aspects of acute and chronic pain”. - Nizhny Novgorod, 2003. - pp. 113–115.
10.Orlova O.R. Focal dystonia: clinical picture, pathogenesis, treatment using botulinum toxin. Dissertation for the degree of Doctor of Medical Sciences. - Moscow, 2000. - pp. 13–29.
11.Orlova O.R., Yakhno N.N. The use of Botox (botulism toxin type A) in clinical practice. - M., 2001. - P. 143–147, 161–163.
12. Orlova O.R., Mingazova L.R., Vein A.M. Myofascial pain syndrome of the face: new aspects of the clinic, pathogenesis and treatment // New in dentistry. - 2003. - No. 1. — pp. 25–29.
13.Petrov E.A. Electrophysiological characteristics of pain syndrome of temporomandibular joint dysfunction // Ross. dental magazine. - 2002. - No. 6. - P. 34–35.
14.Petrosov Yu.A., Skorikova L.A. Prevention of TMJ dysfunctions by eliminating parafunctions of the masticatory muscles // Abstracts of the V All-Russian. Congress of Dentistry: Prevention of dental diseases. - Novosibirsk - M., 1988. - P. 156–157.
15.Al-Ahmad HT, Al-Qudah MA. The treatment of masseter hypertrophy with botulinum toxin type. — A. Saudi Med. J. - 2006. - 27. R. 397–400.
16.Gurney CE Chronic bilateral benign hypertrophy of the masseter muscle //Am. Surg. - 1947. - No. 73. - P. 137.
17.Moore AP, Wood GD The medical management of masseteric hypertrophy with botulinum toxin type A // Br. J. Oral Maxillofac Surg. - 1994. - No. 32. - P. 26–28.
18. Sannomiya E., Goncalves M., Masseter muscle hypertrophy // Bras. Dent. J. - 2009. - No. 17 (4). — R. 347–350.
19. Slavicek R. The masticatory organ: Function and Dysfunction.
— Kloster neuburg: Gamma Med. — wiss. Fortbildungs - GmbH, 2006. - R. 59–90. toxin type A // Saudi Med. J. - 2006. - No. 27. - P. 397–400. come back